Fractures of the carpal bones are rarely diagnosed; most commonly, the metacarpal breaks in two. The fracture is often accompanied by a dislocation. False joints and cysts often form in the bone at the fracture site. The duration of immobilization is 1-6 months.
- construction of the hand
- Anatomy of the hand skeleton:
- The effects of the treatment are:
- Causes of hand fractures
- Symptoms of a hand fracture
- Fractures of the carpal bones
- Fractures of the navicular bones
- Metacarpal fractures
- Fracture of the first metacarpal
- Removal of spokes and wire after Weber patella osteosynthesis
- Plate removal after surgery
construction of the hand
The bones of the wrist, metacarpals, and phalanges make up the skeleton of the hand. These bony structures are fused together by various types of joints. The long and short (intrinsic) muscles of the hand are connected by tendons to the bony structures of the hand and enable the unique movements of the fingers and hand as a whole. In addition to these three main bone groups, the hand skeleton contains sesamoid bones.
The hand mediates human interactions with the outside world. She can signal the presence of common illnesses and bad habits in a person. Examination of the hand not only provides information about local changes, but also about the condition of the entire body.
Anatomy of the hand skeleton:
- wrist
- scaphoid
- triquetrum
- sicklebone
- pea leg
- Big polygon leg (trapezium leg)
- Small polygonal leg (trapezoidal leg)
- skull bones
- hook bone
- metacarpals
- finger bones
The skin of the hands is often considered an indicator of age. Studies show that a person's age can be determined by the appearance of their hands with an accuracy of up to five years.
Fullness on the hands leads to an accelerated development of deep wrinkles. Due to external factors such as (UV radiation, chemical influences on the skin, temperature fluctuations, etc.), the first age-related changes in the skin on the hands appear long before the 'crow's feet' and nasolabial folds that many people fear.
This process can be slowed down with timely cosmetic treatments.
biorevitalization – An injection treatment in which hyaluronic acid is injected into the middle layer of skin, which forms the nutrient framework for the top layer of skin.
The effects of the treatment are:
- The skin is visibly smoother and firmer;
- The visibility of veins is reduced;
- pigmentation is smoothed;
- The skin turgor is improved (lifting effect),
- the feeling of dryness disappears.
Sources: https://totispharma.com/, https://virtusclinic.ru/, https://leyla-roz.ru/, https://skin.ru/, https://virtusclinic.ru/, https:/ /meduniver.com/, https://www.elib.vsmu.by/
Causes of hand fractures
- Fall onto an outstretched upper limb
- heavy push
- car accident
- Sports or work-related injuries
The broken hand bones may or may not be displaced. An open injury is characterized by a wound surface with protruding bone fragments. More common closed injuries are characterized by the absence of a superficial wound. The integrity of the joints can be compromised by the fracture.
Symptoms of a hand fracture
Depending on the area of damage, this disease has a different appearance and is accompanied by specific symptoms. For example, if the scaphoid, triquetrum, and crescent bone are damaged, mobility of the upper limbs in the wrist is reduced because these anatomical structures are part of the wrist. The main symptom is a pain syndrome. The pain can occur at rest and increases with movement.
- acute pain when touching the hand or wrist
- Deformation of the fingers with limited motor skills
- Sensation of a bone fragment in the area of the anatomical snuff box at the base of the thumb
- swelling, bruising
It is difficult to identify the affected area and differentiate between a fracture and an anatomical disorder based on symptoms alone. The doctor uses this information to make an initial diagnosis. Objective investigations are required to identify the affected anatomical structures.
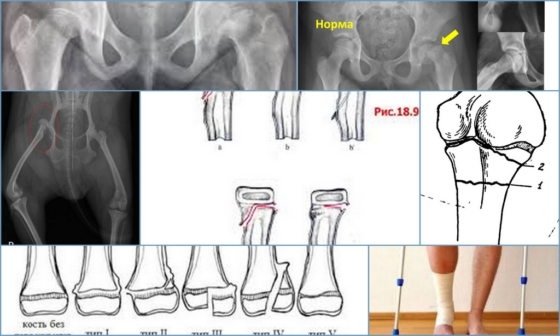
Fractures of the carpal bones
Because of their shape, structure, and location, the carpal bones rarely break. The scaphoid — the large bone at the base of the thumb — is most commonly affected by fractures. Fractures of the crescent and pea bone of the wrist are also common. The triangular bone and the bones of the distal row - the polygonal, trapezoidal, parietal and hamstring bones - are extremely rare and are usually associated with dislocations of the corresponding joints.
Fractures of the navicular bones
Caused by a flexed-hand fall, a punch, or direct trauma to the wrist. Possible variants are:
- Intra-articular fracture of the scaphoid – the fracture line is within the joint cavity of the wrist;
- Extra-articular fracture – a tear in the navicular bone;
- De Kerwen fracture – simultaneous fracture of the navicular bone and displacement of its proximal fragment and carpal bone from the carpal joint.
Symptoms include pain and swelling at the base of the thumb, an inability to move the hand in the wrist, and an inability to make a fist. The diagnosis is made based on the patient's symptoms, the nature of the injury, examination, and X-rays of the carpal bones. If there is no displacement of the fragments, sometimes the line of fracture cannot be determined with all the signs. In this case, immobilization is maintained, and X-rays are repeated after 7-10 days, when the fracture line becomes clearly visible due to the activation of the regenerative processes.
Treatment consists of immobilization with a cast for 4 weeks, followed by monitoring and prolongation of immobilization if fracture consolidation is insufficient. In the case of displaced fractures and fracture detachment, closed reduction is ineffective and immobilization of scaphoid fractures with a spoke is indicated. Fractures of the heel bone are often complicated by the formation of a false joint or lysis of the bone fragments due to damage to the blood vessels that supply them during the injury. That is why it is so important to follow all the doctor's instructions and take x-rays in a timely manner in order to avoid complications and deterioration in the functioning of the wrist. After metacarpal repair, physiotherapy and physical therapy are indicated to restore wrist function.
Metacarpal fractures
The long and slender metacarpal bones are commonly fractured from a punch or as a result of direct trauma. Muscle tension and hand movements prior to fracture immobilization often result in displacement of the bone fragments. A distinction is made between epiphyseal fractures, where the fracture line is in the area of the bone heads, and diaphyseal fractures, where the bone shaft is broken.
Fracture of the first metacarpal
Caused by a bent first finger, more rarely by a direct blow to the first metacarpal.
Fracture of the base of the first metacarpal. A typical injury in boxers and MMA fighters. A distinction is made between a Bennett fracture, in which the base of the first metacarpal, which is held by ligaments, is torn, and a simultaneous dislocation of the large metacarpal in the carpal joint. The Roland fracture is a multiple fracture of the first metacarpal. Both injuries present with pain, deformity and swelling in the 'anatomical snuffbox' - the area under the base of the first finger - with increasing pain with movement and attempting to clench a fist. Diagnosis is based on symptoms, history of injury, examination of the area of injury, and X-rays of the hand. Bennett and Roland fractures are treated surgically with osteosynthesis, that is, the integrity of the bone is restored by fixing the fragments with metal pins, pins or plates.
Fracture of the middle part of the first metacarpal. Most often it is caused by a direct blow to the bone. It manifests itself as pain, swelling and deformation in the area of the first metacarpal. The diagnosis is made based on the patient's complaints, information about the mechanism of injury, examination of the first metacarpal, and x-ray of the hand bone. Treatment consists of cast immobilization for 4-5 weeks; if the fragment is displaced, a closed reduction is performed first. If conservative repositioning is ineffective, an operation is performed to reunite the fragments – spiral osteosynthesis.
Example of one by Dr. Valeev performed surgery to heal a fracture of the first metacarpal:
Removal of spokes and wire after Weber patella osteosynthesis
In the case of kneecap fractures with dislocation, osteosynthesis, i.e. the fixation of bone fragments, is carried out in order to restore the integrity of the bone and thus the function of the knee joint. If the operation is refused, there is a risk that the patient will remain disabled.
In most cases, the Weber technique is used for patellar osteosynthesis. Two titanium Kirschner pins are attached to the bone fragments and clamped together with a titanium wire 8 . In this way, the damaged bone can be restored quickly and very effectively, and - just as important - the metal construction is very inexpensive. However, it has one major disadvantage. Very often patients experience discomfort and pain in the bone and wire area because the wire is just under the skin. For this reason, the metal structure is often removed from the kneecap.
Once the bone has healed and the steel structure has served its purpose, it can be removed. Complete healing of the bone occurs within 6-8 months, in some cases up to a year. The metal can only be removed after this time.
The usual blood tests must be carried out before the operation; a list of these examinations can be found here.
The operation is often performed in a day center, so the patient can go home just a few hours after the operation. Anesthesia is local, either through a wire or through anaesthesia. The operation itself takes about 30 minutes. Locating the wire and spokes is usually not difficult for the surgeon. Once the metal structure is removed, the wound is stitched and an aseptic bandage applied. The patient is bandaged for the first 24 hours, after which he can look after himself or be treated at a hospital near where he lives. The sutures should be removed 14 days after the operation. Painkillers and antimicrobial drugs are administered in the early postoperative period.
Plate removal after surgery
Plates and screws fix almost all bones in the human body. It is a very safe and convenient method of osteosynthesis. There are now a large number of plates of different shapes, sizes and modifications for each type of fracture. The most common examples of plate osteosynthesis are:
- osteosynthesis of the clavicle;
- Osteosynthesis of the humerus
- osteosynthesis of the lateral malleolus;
- Internal fixation of lower leg fractures;
- Osteosynthesis of the metacarpal and metatarsal bones;
- Osteosynthesis of the radius and elbow bones.
- metatarsal and metacarpal bones.
- Fracture of the calcaneus of the foot.
- Bone structure of the navicular foot.
- Shoe prophylaxis - what is it?.
- fracture of the elbow in the foot.
- Complete separation of the articular ends of the bones.
- tibia and fibula.
- The sit bones.
