Important: The elephant's foot disfigures the limbs and causes severe psychological trauma. Therefore, it is advisable to also pay attention to the patient's emotional state.

- Elephantiasis: causes, symptoms, treatment, prevention
- signs and symptoms
- Which organs can be affected by elephantiasis?
- pathogenesis
- Causes of elephantiasis on the legs
- classification
- Causes of Lymphedema.
- causes
- symptoms of the disease
- complications
- Treatment of lymphedema
- Prognosis of filariasis
- General principles of drug therapy
- Effectiveness of medications against lymphatic congestion
- Treatment of elephantiasis
- Conservative therapy
- surgical treatment
- prognosis and prevention
- Treatment of hereditary lymphedema
- prognosis and prevention
Elephantiasis: causes, symptoms, treatment, prevention
Elephantiasis, also known as elephantiasis, is a rare disease. It is most often diagnosed in people from tropical countries where the pathogenic filarial worms occur. Elephantiasis occurs in 90 percent of patients, rarely on the face, genitals, arms and breasts. The affected parts of the body grow to enormous size, the lower limbs become elephant-like, hence the name.
elephantiasis (also known as elephantiasis, elephantiasis, elephantiasis) is a disease characterized by severe enlargement of body parts, especially the limbs (legs, arms). Other areas commonly affected include the external genitalia. Elephantiasis results from an obstruction (blockage) of the lymphatic system, which leads to a buildup of fluid, lymph, in the affected areas.
The lymphatic system is part of the immune system and helps protect the body from infection and disease. The lymphatic system consists of a network of tubes (lymphatic vessels) that drain a thin, watery fluid called lymph from various areas of the body into the bloodstream. Blockage of these vessels initially causes lymphedema (usually in the legs or arms) and can gradually lead to massive swelling and general enlargement of the body parts that are characteristic of elephantiasis.
The most common cause of elephantiasis is a parasitic disease known as lymphatic filariasis. The lymphatic system damage associated with elephantiasis also has other causes, including some sexually transmitted diseases (e.g., venous lymphogranuloma); Tuberculosis; an infectious disease called leishmaniasis; recurrent streptococcal infections; Leprosy; and environmental factors such as exposure to certain minerals (e.g., silicon dioxide). In some cases, the cause of the disease cannot be determined (idiopathic).
signs and symptoms
The main symptom of lymphatic disorder is mild swelling, which, if left untreated, can gradually develop into elephantiasis.
The main symptom of elephantiasis is significant enlargement and swelling of an area of the body due to fluid buildup. The arms and legs are most commonly affected. An entire arm or leg can enlarge many times its normal size, resembling the thick, round shape of an elephant's leg (see 'Elephant Leg'). photo above). The skin in the affected areas is usually dry, thickened, scaly and may become pitted, bony and dark (hyperkeratosis). Fever, chills and general malaise may also occur.
Elephantiasis can also affect the external genitalia of men and women. In men, the scrotum may be enlarged, and the penis may be pulled under the skin, appear thickened, inflexible, warm, and painful. Thickening of the vas deferens may occur. Those affected may experience pain and burning.
The external parts of the female genitals (vulva) can also be affected by elephantiasis. A swollen mass with thickened and ulcerated skin may form between the thighs and may be accompanied by enlarged lymph nodes (lymphadenopathy) in the legs. Some women may experience enlarged breasts.
Damage to the lymphatic system can lead to susceptibility to secondary bacterial and fungal infections, which can significantly worsen the condition. Although the legs, arms, and external genitalia are most commonly affected, elephantiasis can affect any area of the body.
Which organs can be affected by elephantiasis?
Elephantiasis usually affects the patient's limbs. In the early stages of the disease, only a slight swelling is noticeable, which occurs in the evening and disappears after a massage. As the disease progresses, the limbs change shape, increase in volume, and the proportions become abnormal.
pathogenesis
Elephantiasis begins with mild swelling and swelling that can come and go. Eventually, after about 1-3 years, there is a two- or three-fold thickening of the lower extremity and possibly the thigh if the leg is affected. The shape of the leg is abnormal, cylindrical and thickened, e.g. B. the ankle joint may be flattened.

The mechanism of excessive thickening of the affected parts is due to congestion affecting the lymphatic system. These can be caused by the following factors, among others:
- Blockage of the lymphatic vessels by parasites – e.g. b. Roundwormssuch as roundworms, Filariae, Chyluria Etc;
- Suppuration and subsequent scarring of lymph glands, e.g. B. the inguinal glands;
- lymphangitis Lymphangitis, Phlebitis, corneavaricose ulcers, chronic eczema, syphilis, LupusIn case of repeated frostbite and other chronic or recurrent processes leading to inflammatory edema.
The resulting lymphatic stasis leads to infiltration of lymph into the tissue gaps and overnutrition of the adjacent tissue structures, leading to hyperplasia due to connective tissue hypertrophy in the subcutaneous tissue. This process is chronic and takes many years to develop, which is why it is rare in adolescents.
Warning!!! Vucheriosis and other filariasis are caused by parasitic, very thin worms (maximum 0.3 mm in diameter and up to half a meter long) that can block the lymphatic system. They are transmitted and spread by blood-sucking insects, so when vacationing in tropical countries you should definitely protect yourself with repellent and mosquito nets, as they not only cause elephantiasis, but can also penetrate the eyes, which can lead to Blindness.
Causes of elephantiasis on the legs
There are two main causes of elephantiasis:
- congenital or acquired disorders of the lymphatic system, including overproduction of lymph, malformations, aplasia, valvular insufficiency, stenosis and occlusion of the lymphatic vessels, as well as diseases such as. Nononne-Milroy syndrome, Schereshevsky-Turner syndrome;
- Infectious agents, often parasites, which include. Bancroft nematode - caused Vucherriosisbut can also be caused by streptococci;
- mechanical injuries and thermal burns (frostbite is most common);
- neoplastic growths that can compress lymphatic vessels;
- Iatrogenesis – can be caused by radiation or surgery;
- Circulatory disorders – chronic venous insufficiency i post-thrombotic syndrome;
- Central nervous system disorders;
- endocrine disorders.
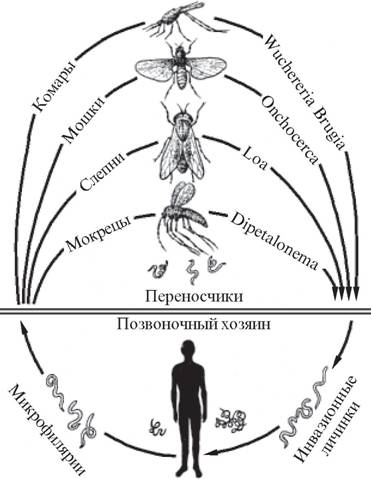
Life cycles of the different filarial species
Elephantiasis, caused by various parasitic roundworms (filariosis), is more common in tropical areas (Indian Archipelago, Arabia, West Coast of Africa, Central America), where mosquitoes spread and transmit the infection. It is very rare in the former CIS countries.
classification
There are several stages in the development of lymphedema:
- Stage I is characterized by early accumulation of fluid containing a lot of protein. At this stage, edema develops, which is relieved by elevating the limbs. After compression, traces of swelling may remain. During this time, the number of different proliferating cells increases.
- In the second stage, the edema does not go away when the limb is elevated. In this position, pressure marks remain. At a later stage of this stage, persistent edema occurs, Hyperplasia of fatty tissue i Fibrosis.
- Third stage – lymphatic elephantiasis is detected, in which no traces of pressure remain. Trophic skin disorders, fibrosis and fatty deposits may develop.
Depending on the characteristics of the physiological changes, a distinction is made between primary and secondary lymphatic insufficiency:
- Primary (congenital) – develops as a result of congenital anomalies of the lymphatic system. In congenital anomalies, abnormal lesions may occur in one or more limbs. Symptoms can occur both in adulthood and in childhood. In rare cases, the form is also hereditary. Statistically, this form is diagnosed in 6 % of all cases of lymphostasis.
- Secondary (acquired) – the disease can develop after trauma, surgical intervention, other diseases and unfavorable factors affecting lymphatic flow. The secondary process usually affects a limb. The lower limbs are most commonly affected.
Depending on the age at which the patient develops lymphedema, the following forms are distinguished:
Causes of Lymphedema.
The causes of lymphedema are often the following:
- Infectious diseases that trigger the development of inflammatory processes in the skin and subcutaneous tissue.
- thrombophlebitisi varicose veinsInfectious diseases leading to chronic venous insufficiency syndrome.
- Burns and injuries in which the subcutaneous cell layer is damaged.
- Narrowing of ducts, damage to lymph nodes.
- Cancer diseases and their treatment radiotherapy.
- Parasitic damage to the structures of the lymphatic system.
- Kidney and heart diseases.
The influence of these factors, combined with certain body characteristics, leads to a violation of the contractile and conductive function of the lymphatic vessels. As a result, lymphedema develops in the legs or arms. However, lymph flow disorders are particularly dangerous for the lower limbs because they absorb a lot of lymph fluid due to gravity.
Lymphatic congestion in the hand after breast removal develops as a result of significant disorders in the body. After the breast and thus the lymph nodes are removed, lymph fluid accumulates in the shoulder and forearm, which leads to the development of edema. In fact, the lymphedema is after Mastectomy can manifest months or even years after surgery. Statistically, it occurs in about a quarter of all women who have had surgery.
causes

Lymphatic stasisAs with many diseases, elephantiasis does not occur without pre-existing pathologies or other disorders. Lymphatic congestion can occur due to a narrowing or blockage of the ducts. The disease can develop against the background of rusty inflammation of the lower limbs. Namely, with this pathology, the patient has skin lesions through which pathogenic bacteria penetrate and then spread in the lymphatic vessels, causing inflammation and structural changes. As the disease progresses, the vessel walls thicken so that the fluid can no longer circulate properly.
The pathology can develop after an operation to remove lymph nodes. Such operations also affect fluid circulation. A problem can arise with parasite infestation, but in this case the helminths must penetrate the body and affect the lymphatic vessels. It can also occur in people who have metastatic cancer, which tends to spread to a lymph node or vessel.
symptoms of the disease
Let's consider the symptoms typical of the disease. There are three stages of the disease:
- Mild. Occurs when the disease has not yet had time to develop. The swelling occurs, subsides spontaneously and later progresses to a persistent stage.
- Mixed. Occurs only on the periphery of the limbs.
- Firmly. When general fibrosis of limb tissue develops. The edema itself can be discovered completely accidentally, e.g. B. by simply going home and stretching your legs.
What is characteristic of the disease is that the swelling spreads from the foot or ankle upwards and can affect the entire leg. The swelling remains a symptom even after a long time, and the cause of the disease is the strain on the leg. The swelling disappears or decreases significantly when the affected person rests.
At this stage of the disease, the affected person suffers from fatigue and discomfort in the limbs, the tissue of which is characterized by a loose, doughy texture. The skin is usually unchanged; mechanical impact on the skin causes small depressions, the cause of which is a disruption in cell turgor. If action is not taken decisively, the swelling will continue and gradually increase. The limb becomes ugly and looks like an elephant leg. At this stage, there is no pain, and the skin surface is smooth and slightly yellowish, lemon-yellow in color. Heavy sweating, which contributes to inflammation, rarely occurs. The sensation remains unchanged. Cutaneous sensitivity in elephantiasis of the feet is more often preserved.
Swelling due to venous insufficiency and obesity must be differentiated from the disease. In elephantiasis, the limbs are disfigured by rough wrinkles. In the initial phase, diagnosis is very difficult if the person has comorbidities.
complications
In lymphedema, tissue nutrition is impaired. Areas of hyperkeratosis form. The changed skin dissolves and ulcers form. Lymphatic fistulas sometimes form between the fingers. Lymphedema of any origin is often complicated by a rust infection, which can cause mucus, causing the obstruction of the congested lymphatic vessels and leading to rapid progression of the disease. Lymphangiosarcoma can develop over the long-term course of the disease (particularly in secondary lymphedema).
The diagnosis is made by the phlebologist based on the external examination, measurement of the limbs and the anamnesis. Lymphangiography is used to assess the condition of lymphangiomas (small lymph vessels). If the lymphogram shows bulging or spindle-shaped vessels, motility is preserved. If a vessel is evenly filled with contrast medium and its diameter is the same along its entire length, this indicates normal permeability with damage to the contractile apparatus and impaired lymphatic transport. In primary lymphedema, hypoplasia of the lymphangia is noted; With secondary edema, changes in the shape of the vessels, extravasation and filling of the cutaneous lymphatic network are noted.
Lymphoscintigraphy is used to examine the dynamics of the disease. The nature of the isotope distribution allows assessment of main, diffuse and collateral lymphatic flow and detection of complete lymphatic stasis. In recent years, lymphangiography has gradually been replaced by new examination methods. Magnetic resonance imaging, computed tomography, and duplex scanning are increasingly used to assess lymphatic flow and the condition of the lymphatic system.
Lymphedema must be differentiated from edema due to postthrombotic syndrome, kidney or heart disease. If primary lymphedema is suspected, the differential diagnosis of lipedema (morbid leg obesity syndrome) should be made. In contrast to lymphedema, lipedema is characterized by symmetrical involvement of the lower limbs. The feet remain unaffected.
Treatment of lymphedema
Conservative treatment is possible if there are no organic changes in the soft tissues. Patients are prescribed a special diet, physical therapy, balneological and physiotherapeutic treatments. Bandages, massage with lymphatic drainage, and alternating pneumocompression devices are indicated to reduce the volume of the affected limbs. The comprehensive treatment methods of modern phlebology make it possible to slow down the development of lymphedema and, in some cases, even achieve a regression of the symptoms of the disease.
Lymphatic bypasses are created through surgical procedures. The lymphatic vessels are stained beforehand. During the operation, the largest number of vessels are marked in the popliteal fossa or in Scarpa's triangle on the thigh. The vessels are divided and their central ends are coagulated. Anastomoses are then created between the peripheral ends of the vessels and the nearest branches of the great saphenous vein. If carried out early, the operation allows for complete normalization of lymphatic drainage. In the long term, a significant reduction in swelling of the skin and subcutaneous tissue can be achieved after the operation.
Prognosis of filariasis
The prognosis of filariasis is good if the infection is diagnosed and treated early. Filarial disease is rarely fatal, but the consequences of the infection can cause significant personal and socioeconomic problems for those affected.
The occurrence of filariasis in humans is mainly due to the host's response to microfilariae or the development of adult worms in different regions of the body. In rare cases, long-term disability can occur due to chronic damage to the lymphatic system or blindness, depending on the infectious filarial organism.
I am concerned with the prevention and treatment of coloproctological diseases. Higher medical education. On the website tvojajbolit.ru I will be responsible for the quality and literaryness of the articles.
Specialty: phlebologist, surgeon, proctologist, endoscopist.
General principles of drug therapy
Lymphostasis of the upper and lower extremities is treated with massage, therapeutic exercises and physiotherapy. In addition to medications, the patient must wear compression clothing and follow a diet.
Conservative treatment methods are particularly effective in the early stages of the disease, when the skin and connective tissue have not yet been pathologically attacked.
In severe cases, surgical treatment may be necessary. Drug treatment depends on the underlying cause of the disease.
The most commonly prescribed medications include venotonics, diuretics, angioprotectors, homeopathy, antibiotics and enzymes. As a rule, these are systemic and topical medications:
| Pharmacological group. | Name of the drug | Effect on the body |
| Venotonics | Detralex, Diosmin, Venodiol | Restoration of lymphatic drainage |
| Diuretics | Furosemide, torasemide, licorice root | Drain excess fluid from the body. |
| Angioprotectors | Phlebodia, Troxerutin | Protect the vein walls and make them more flexible and plastic. |
| homeopathy | Lymphomyozot | Lymphatic cleansing, removal of toxins. |
| Enzymes and coumarins. | Wobenzym, Flogenzym, Neodicumarin | Reducing inflammation, improving blood flow |
While taking the medication, patients should not bathe or go to the sauna as evaporation impairs lymphatic and blood flow. Avoid sitting in the same position for a long time with one foot on the other or walking barefoot on the street, as there is a high risk of damaging the feet and developing purulent sores. Experts also advise against wearing uncomfortable high-heeled shoes and wearing tight synthetic underwear. The use of talc and powder to reduce foot sweat, timely trimming of nails, and the use of lotions and oils during water treatments are recommended.
Effectiveness of medications against lymphatic congestion
To prevent lymphatic congestion after surgery, LFC is recommended with gymnastic exercises, massage of the upper and lower limbs and physiotherapy. The patient should avoid unhealthy habits, heavy physical exertion, hypothermia and trauma. The use of topical and systemic medications, including antiseptic creams, ointments, and gels, is important.
Pharmacotherapy includes the administration of broad-spectrum antibiotics, analgesics, nonsteroidal drugs, diuretics, angioprotectors, venotonics, enzymes and coumarins. Immunomodulators and antihistamines are also prescribed. Wound-healing, antiseptic ointments should be applied to the affected skin.
Treatment of elephantiasis
Conservative therapy
Non-surgical treatment is prescribed alone if the patient's condition is satisfactory and there are no serious tissue changes, or as an adjunct to surgical correction in the pre- and postoperative periods. Conservative treatment of elephantiasis is complex, carried out continuously and includes 3 main directions:
- Mechanical methods. To improve lymphatic drainage, compression therapies with elastic bandages and special fabrics, lymphatic massages and physiotherapy are used.
- physical therapy. Physiotherapeutic treatments act on the pathological part of the lymphatic system and provide long-term results. Intermittent pneumatic compression, ampoule therapy, laser therapy and photodynamic therapy are used in the treatment of elephantiasis.
- Pharmacotherapy. Pharmacotherapy is divided into traditional treatment with phlebotonics, vitamins and diuretics as well as newer forms of treatment with benzopyrones and enzyme preparations.
surgical treatment
Most patients require surgical correction of lymphatic drainage over time. Lymphatic anastomoses are placed to bypass lymphatic drainage into the venous system, and the operation is performed using microsurgical techniques. In case of irreversible structural changes in the limbs, the only treatment is skin plastic surgery, which partially restores the function of the limbs.
prognosis and prevention
Psoriasis is not a fatal disease, but it causes permanent tissue changes and becomes a cause of disability. The prognosis depends on correct diagnosis and treatment. To prevent the disease, it is recommended to increase daily physical activity and enrich the diet with antioxidant, vitaminized products. Compression stockings for the legs are recommended when standing or sitting for long periods of time.
3 Lymphedema of the lower limbs: diagnosis and treatment algorithm / OV Fionik // Surgical News. – 2009. – №4.
4. lymphedema (elephantiasis) of the lower limbs (etiopathogenesis, clinic, treatment)/ NP Snytko // Bulletin of the Smolensk Medical Academy. – 2003. – №1.
Treatment of hereditary lymphedema
Therapy of hereditary lymphedema is based on several principles - improving lymphatic drainage, reducing fluid accumulation in tissues and eliminating secondary disorders arising from the edema syndrome. To improve lymphatic drainage, various lymphatic drainage massages (both manual and mechanical) and special compression stockings are used, and local medications are sometimes administered. For some forms of hereditary lymphedema, surgical techniques that allow more complete drainage of tissue fluid into the lymphatic system or circulatory system may be effective. Special diets with reduced protein and salt are prescribed to reduce lymphatic congestion in tissues - these nutrients can significantly worsen lymphedema.
In advanced forms of hereditary lymphedema with severe secondary diseases (elephantiasis, trophic ulcers, infections), complications are treated. To combat infections, antibiotics are prescribed, trophic disorders are treated with vitamins, regenerative agents and biogenic stimulants. In severe elephantiasis, surgical removal of excess tissue volume is sometimes performed (resection surgery), which improves both the appearance and condition of the patient with hereditary lymphedema.
prognosis and prevention
The prognosis of hereditary lymphedema depends on the severity of symptoms, timeliness of treatment and many other factors. Under optimal conditions, that is, with regular massage with lymphatic drainage, proper nutrition, limited fluid intake and physical activity, the prognosis is quite favorable - patients may only be bothered by swollen feet at the end of the day. If hereditary lymphedema is severe, if the treatment plan is not followed or treatment is not carried out, the disease can lead to disability due to elephantiasis and even death due to secondary infections and trophic disorders. Patients should therefore carefully follow all recommendations, avoid salty or high-protein foods, maintain a drinking regime and avoid prolonged strain on the limbs, especially of a static nature, if they are ill.
1. Lymphatic outflow disorders: lymphostasis, lymphedema: a textbook/ SA Alexeev, PP Koshevsky. – 2016.
2. Treatment of lymphedema of the extremities (literature review)/ Yudin VA Savkin ID // Pavlov Russian Medical and Biological Bulletin. – 2015.
3. Lymphedema of the lower extremities: diagnosis and treatment algorithm / Fionik OV, Bubnova NA, Petrov SV, Erofeev NP, Ladozhskaya-Gapeenko EE, Semenov A.Yu. – 2009.
Read more:- What is elephant foot disease?.
- Why the legs are longer than the body.
- foot of phot.
- Anatomy of the ligaments of the lower limbs.
- Shoes for swollen feet.
- The tarsal of the foot.
- How to enlarge the foot.
- Pain in the periosteum of the tibia.
