Equinovarus is a severe foot deformity in which the bones of the foot are deformed and repositioned, affecting muscles, ligaments, blood vessels, and nerve endings. It causes a gait disorder and affects the entire musculoskeletal system.

- Tendon transfers to correct spastic varus foot deformity: a case series report
- methods
- Results
- conclusion
- Introduction
- clubfoot
- Classification of clubfoot
- clubfoot
- Methods for diagnosing clubfoot
- Advanced treatment for congenital foot deformities in infants
- Before and after treatment
- Treatment of forefoot shortening (varus)
- WITHOUT plaster
- Information for Parents
- clubfoot
- flat feet
- Clubfoot (Calcaneovalgus Clubfoot)
- clubfoot
- Treatment methods for valgus foot in children and adults
- Prevention of clubfoot
- Features of a flatfoot deformity
- Features of equinovarus foot deformity
Tendon transfers to correct spastic varus foot deformity: a case series report
Overactivity of the tibialis anterior and/or posterior muscle tendons may be a causative factor in spastic varus foot deformity. The prevalence of this dysfunction has been described, but the results are not well defined. Although gait analysis and dynamic electromyography provide useful information for patient assessment, they are not available in every hospital. The aim of the present study is to identify the muscle causing the deformity and to apply the most appropriate technique to correct it.
methods
We retrospectively studied 48 consecutive patients (52 feet) with spasticity due to cerebral palsy. The mean age at surgery was 12.4 years (9-18 years) and the mean follow-up was 7.8 years (4-14 years). Eigtheen's feet exhibited an equatorial hindfoot deformity resulting from shortening of the gastrocnemius and soleus muscles. Depending on the deformity, the feet were divided into two groups (group I with forefoot and midfoot inversion and group II with hindfoot inversion). The deformities were flexible in all cases in both groups. Split anterior tibial tendon transfer (SPLATT) was performed in group I (11 feet) and split posterior tibial tendon transfer (SPOTT) in group II (38 feet). Both procedures were performed on three feet. Achilles tendon lengthening using the gliding method (Hoke method) was performed on 18 feet preoperatively or at the same time as the index method.
Results
Group I results were rated excellent according to Hoffer's clinical criteria for 8 feet and fair for 3 feet, while group II results according to Kling's clinical criteria were excellent for 20 feet, good for 14 feet and good for 14 feet 4 feet were rated as bad. The feet with poor outcomes had residual varus deformity due to intraoperative technical errors.
conclusion
Overactivity of the anterior tibialis tendon causes inversion, which is most pronounced in the forefoot and midfoot. In some cases where Achilles tendon shortening is associated with a valgus foot, the deformity may not be clinically evident. By identifying the muscle causing the deformity and applying an appropriate technique, very satisfactory results have been obtained in most cases. With three feet, both muscles contributed to the combined deformity, so performing SPLATT and SPOTT simultaneously was deemed necessary. For complex foot deformities where a cavus component is present, complementary treatments are required along with index surgery to achieve the best outcome.
Introduction
Varus foot is often a result of cerebral palsy. Procedures to transect the anterior (SPLATT) or posterior (SPOTT) tibialis tendon are often performed to correct this deformity. In both procedures, the distal portion of the tendon is split longitudinally, half of the tendon is detached from its medial insertion and reattached on the lateral side of the foot [1]. The aim of semi-transposition is to act on the muscle-tendon complex in such a way that there is neither inversion nor evertation of the foot, thus maintaining stability and flexibility.
The Hoffer et al. The SPLATT described in [2] corrects the supination and deformity of the varus-metatarsus resulting from spasticity of the anterior tibialis muscle. Hindfoot equinovarus is most common in children with spastic hemiplegia and is caused by spasticity of the posterior tibial muscle, which is very commonly combined with peroneal muscle weakness and heel bone tension [Figure 1].

The reported clinical outcomes of SPLATT and SPOTT were generally good but very different [2-9]. The SPLATT was first used by Kaufer et al. [10] and by Green et al. [4] and Kling et al. [6] was popularized as a technique to balance the hindfoot and preserve plantar flexion strength, but should only be used in patients 4 to 6 years of age because of the potential risk of foot conversion to a valgus deformity in children under 4 years of age. A prerequisite for a tendon split transfer is the ability or potential ability to walk. A contraindication is a fixed bone deformity and a severe contracture, affecting mainly the anterior part of the tibia, since the transferred semitendon cannot reach the elbow bone.
clubfoot
clubfoot (equinovaristic foot deformity) is one of the most common musculoskeletal abnormalities (33-38 %). It usually occurs bilaterally. Clubfoot is twice as common in boys as in girls.
The causes of the development of clubfoot are not fully understood. Modern traumatology and orthopedics indicate that risk factors for developing clubfoot include fetal deformities, lack of amniotic fluid, smoking, and alcohol and drug use. The development of the foot bones, muscles and nerves of the lower leg is affected by fetal malformations. Secondary clubfoot can occur due to pathology in other parts of the musculoskeletal system.
Classification of clubfoot
- Idiopathic clubfoot. It is characterized by a drop in the waist associated with an abnormal position of the neck, an imbalance in which the heel is elevated and the foot is bent towards the sole, an abnormal position of the forefoot in relation to the hindfoot, abnormal development of the articular surfaces of the foot, shortening of the calf muscle and abnormal development of the tibial vessels in the forefoot.
- Postural (positional) clubfoot. The bones of the heel and talus are unchanged. The articular surfaces are normally developed and subluxated.
- Congenital clubfootCombined with congenital neuropathy with imiopathy. The foot deformity is secondary to other parts of the musculoskeletal system (multiple limb curvatures, bilateral hip dislocation, etc.).
- Syndromic clubfoot. Combination of the previous form of clubfoot with post-inflammatory abnormalities (amniotic ligaments, renal abnormalities, etc.).
Congenital clubfoot has a balance position, varus position (foot flexed, toes pointing in), and supination (foot with the sole up and pointing in). The mobility of the ankle is restricted.
Because of this change in foot position, the child with clubfoot does not support itself on the sole of the foot when walking, but on the outer edge of the foot. A peculiar gait pattern develops, in which the affected person steps on the supporting leg with every step.
This condition worsens over time. The bones of the foot deform more and more and the ankles become subluxated. The skin on the outer surface of the foot becomes rough. The muscles in the lower legs that are not involved in walking atrophy and the knee joints become dysfunctional.
The later congenital clubfoot is treated, the more difficult it is to repair the damage and restore the shape of the foot.
clubfoot
The sole surface of the foot is turned inwards, which raises the arch of the foot. This deformity usually arises as a result of intrauterine positioning. It usually does not go away after birth and corrective splinting may be necessary.
In flat feet, the normal arch in the middle of the foot appears flattened. All children have flat feet by the age of 3, when the arch of the foot begins to develop. There are two main causes of developing flat feet:
W flat feet Feet stay flat because the arch is very flexible. Flexible flat feet do not require treatment. However, if the child continues to experience pain or cramps in their feet as they age, corrective footwear may be needed.
Z Tarsal charcoal galia The feet are immobilized in a flattened position. The tarsal coalition can be a congenital defect or the result of medical conditions such as trauma or prolonged swelling. Treatment of the tarsal coalition often includes a cast. Sometimes surgical separation of the fused ankle can restore mobility.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Methods for diagnosing clubfoot
It used to be thought that clubfoot was caused by poor posture in the womb. However, in today's technology-intensive medicine, a detailed ultrasound scan can shed light on many questions. Although it is difficult to make an accurate diagnosis due to the baby's position during pregnancy, it is easy to diagnose at delivery. If there are any suspicions, such as B. growth of the foot in the radius, introversion of the big toe, introversion of the heel and downward ankles, a doctor should be consulted for diagnosis. Extended ultrasound examination is required for diagnosis.
As we highlighted above, treatment for Equinovarus foot begins immediately after birth. The treatment process is based on the Ponseti method. This treatment involves pouring the area from the toe to the top of the knee. This is to correct the tendency of the deformity.
This method, which aims to increase the curvature of the sole and turn the foot inwards, requires a period of 6-7 weeks. This last intervention affects the equinus component, ie the height of the heel. Once the cast is removed, the patient must wear special orthopedic shoes. From then on, the patient is observed by a specialist for three months.
Since the ankles of newborns are still soft, it is of great advantage to carry out the necessary interventions without wasting time after the diagnosis. Surgery may be necessary due to aging and loss of ankle mobility. Still, the success rate of equinovarus surgery is quite high.
Advanced treatment for congenital foot deformities in infants



UNFO is a revolutionary solution specifically designed to correct all degrees of congenital shortened feet, also known as varus foot, clubfoot and forefoot adduction in infants and young children.
The UNFO orthosis minimizes the difficulties and stress caused by frequent casts, ineffective stretching and massage, and subsequent under- or over-correction of clubfoot.

Before and after treatment
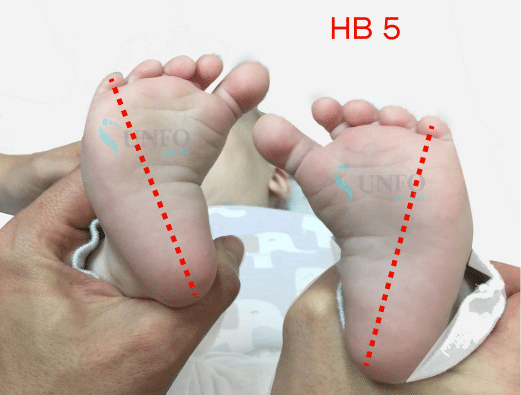

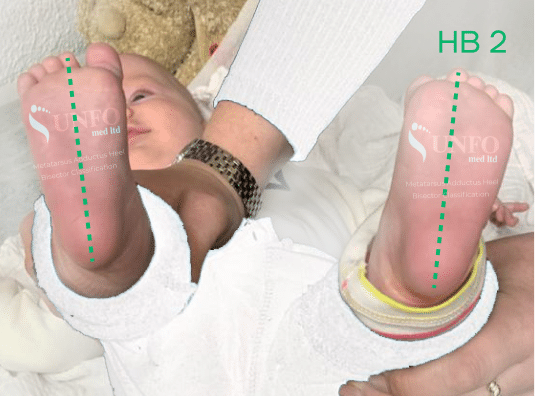

Treatment of forefoot shortening (varus)
WITHOUT plaster
Parents and children around the world can now experience the benefits of UNFO Therapy, which offers an effective and stress-free treatment that relieves family stress and significantly improves quality of life.
Information for Parents

Clubfoot (varus foot, equinovarus, clubfoot, adduction forefoot) is a foot curvature that is common in newborns. Left untreated, this type of abnormality can lead to permanent physical impairment.

The UNFO orthosis meets the highest international medical standards. The effectiveness of the method has been confirmed by scientific studies. Thousands of parents who have chosen UNFO sandals have successfully treated reduced forefoot shortening (clubfoot, forefoot adduction).

clubfoot
In clubfoot, the bottom of the foot is turned inward, causing the arch of the foot to pull up. This defect is usually related to the baby's position in the uterus, does not always resolve after birth, and may require corrective casts.
In heel deformity, the foot is flat or rounded and arched in the plantar direction with the heel pointing outward.
Early treatment with a cast or corrective splint is usually effective.
flat feet
In flat feet, the normal arch in the midfoot area is flattened. Flat feet occur in all children up to the age of about 3 years, after which the arch of the foot begins to form. There are two basic types of flat feet:
W With flexible flatfoot The foot stays flat because the arch is extremely flexible. A flexible flat foot usually does not need treatment. However, if an older child experiences pain or cramps in their feet, corrective footwear may be needed.
If tarsal stiffening The foot is immobilized in a flat position. Tarsal fusion can be a congenital defect, but it can also be the result of a medical condition, such as a heart attack. B. a trauma or a long-standing swelling. The treatment of a tarsal stiffness is often done with a plaster cast. Sometimes foot mobility is restored by surgically separating the stiff joint.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Clubfoot (Calcaneovalgus Clubfoot)
Early treatment consists of fixation (the foot is placed in an equinovarus position) or the use of corrective braces and is usually effective.
The forefoot is rotated toward the midline. The foot may be supinated at rest. In general, the foot can be brought down passively and raised to a neutral position by stimulating the sole. Sometimes the affected legs are stiff and cannot be corrected to the neutral position. Hip dysplasia is more common in these children.
This deformity usually resolves without treatment within the first year of life. If this is not done, splinting or surgery (an abduction osteotomy of the foot) is required.
clubfoot
The sole of the foot is turned inwards, which raises the arch of the foot. This deformity usually results from intrauterine positioning. It usually does not go away after birth, so corrective splinting may be necessary.
In flat feet (flat feet), the normal arch of the foot is flattened in the middle of the foot. All children have flat feet by the age of 3, at which point the arch of the foot begins to develop. There are two main causes of developing flat feet:
W flat feet Feet stay flat because the arch is very flexible. Flexible flat feet do not require treatment. However, if pain or foot cramps appear as the child ages, correction of the footwear may be necessary.
Z Tarsal charcoal galia The feet are immobilized in a flattened position. The tarsal coalition can be a congenital defect or the result of medical conditions such as trauma or persistent swelling. Treatment of the tarsal coalition often involves the use of plaster casts. Sometimes, mobility is restored by surgically separating the fused ankle.
Treatment methods for valgus foot in children and adults
Both conservative and surgical treatment methods are used for clubfoot. An individual treatment plan is created for each patient.
In the case of congenital deformities, treatment should be started immediately after birth. In most cases it is possible to correct the alignment of the foot without surgery until the skeleton is fully ossified.
- foot massage;
- Therapeutic exercise to improve ankle mobility and prevent muscle wasting;
- Gentle immobilization of the foot in a physiological position with special bandages;
- plaster casts (sometimes after correcting the foot with soft immobilization);
- wearing orthopedic shoes;
- Physiotherapeutic treatments.
The same methods are used to treat acquired clubfoot in adults. They are very effective if the disease is diagnosed on time.
If conservative treatment does not help or the patient has a severe form of clubfoot, foot correction is performed surgically. The surgery restores the normal alignment of the foot bones and repairs the foot's ligaments and tendons. In children, this operation is performed after the first year of life.
Prevention of clubfoot
In order to reduce the risk of congenital deformities in children, women during pregnancy are advised to lead a healthy lifestyle, eat a balanced diet and give up unhealthy habits.
To prevent foot deformities in children, it is advisable not to put the child on their feet until the bones are stronger and the child begins to walk independently. It is also advisable to watch the child's gait and go to the pool from an early age.
In addition, it is recommended that both children and adults
- walking barefoot more often on the floor or on a massage mat;
- Wearing shoes that fit well, have a firm heel, and a raised insole on the inside of the foot;
- timely treatment of all infectious and inflammatory diseases.
A consultation with an experienced orthopedic traumatologist in Kiev is possible at the Oxford Medical Center. The clinic has all the prerequisites for diagnosing and treating clubfoot. To make an appointment, call our contact center or use the online chat.
Features of a flatfoot deformity
In clubfoot deformity, the height of the arch of the foot is reduced and the axis is deformed. The midfoot is lowered and the heel and toes are turned outward. The foot looks like the letter X.
This condition causes annoying pain that makes it very difficult to wear shoes. Young children and women over the age of 30 often suffer from this condition. The problem can be effectively addressed by contacting specialists early enough to allow the foot to regain its normal appearance and the joints to function.
If left untreated, a flatfoot deformity can have many negative consequences: a change in the proportions of the articular surfaces, deformation of all toes, a change in gait, pain in the feet, swelling of the limbs, problems with the spine, etc.
Features of equinovarus foot deformity
Equino varus foot deformity is also known as clubfoot. It is characterized by an abnormal position of the foot in which the inside of the foot is raised and arched inward while the outside is sagged. The problem is common in boys.
The equinovarus deformity can appear in several variants. There are congenital, positional, syndromic, and idiopathic forms.
The main treatment methods for clubfoot:
- implementation of phased redress;
- Attachment of prostheses;
- special shoes;
- physiotherapeutic methods;
- use of drugs to block neuromuscular conduction of the calf muscles;
- surgical intervention.
Self-treatment of foot deformities is strictly prohibited, as it can only aggravate the situation. For a successful recovery, the recommendations of the medical specialists must be carefully followed.
Read more:- What is clubfoot?.
- Clubfoot in 7-year-old children.
- equinus.
- Congenital clubfoot.
- Why does a child develop clubfoot?.
- baby splashing.
- Balancing foot alignment.
- Icb varus foot deformity.
