This condition is treated by a neurologist.
- CHERURGIC IMPROVEMENT OF FASSIOPLASTIC WOMAN WITH OSTEOTOMY OF THE EXTERNAL TIBIAL CONDYLE Russian Patent 2018 for MPK A61B17/00.
- Similar patents RU2654593C1
- Causes of Osteophytes
- Symptoms of bony hypertrophy of the articular surfaces
- Causes of osteonecrosis
- risk factors
- Conservative treatment
- pain relief
- causes of injury.
- diagnosis of the injury.
- Functions of the PCC
- Bone contusions and microfractures
- diagnostic procedures
- Physical examination, which includes the following tests:
- Radiological examination.
- Types of aseptic necrosis of the femoral condyle
- symptoms of necrosis
- Home ' How to get there ' Lower Limb Fractures ' Treatment of Fractures of the Tibia ' Treatment of Fractures of the Tibia Condyle.
- symptoms
- diagnosis
CHERURGIC IMPROVEMENT OF FASSIOPLASTIC WOMAN WITH OSTEOTOMY OF THE EXTERNAL TIBIAL CONDYLE Russian Patent 2018 for MPK A61B17/00.
The invention relates to the field of medicine, namely surgery, in particular traumatology and orthopaedics, and is intended for the open repositioning and internal immobilisation of fractures of the lateral condyle of the tibia. Intra-articular fractures of the lateral condyle predominate over fractures of the medial condyle and account for up to 90 % of all intra-articular fractures of the proximal end of the tibia. This type of injury is often accompanied by impingement of the subchondral bone, resulting in a structural defect and dysongruence in the knee joint. The accepted treatment of such fractures is surgery, which involves open reduction, osteoplasty, and rigid immobilization of the fracture with brace plates.
There is a known surgical approach to treating a lateral condylar fracture of the tibia, which involves making a 7-8 cm downward skin incision in the supine position, beginning approximately 1.5 cm medial to the fibular head and 1 cm distal to the popliteal crease. The subcutaneous tissue and the great saphenous fascia are severed sharply. The joint capsule is divided and the knee joint cavity is opened (Liu GY, Xiao BP, Luo CF, Zhuang YQ, Xu RM, Ma WH. Results of a modified posterolateral approach for the isolated posterolateral tibial plateau fracture. Indian J Orthop. 2016 Mar-Apr; 50(2 ):117-22.doi:10.4103/0019-5413.177578).
However, this approach does not provide adequate visibility into the external condyle and requires dissection of the posterior structures, which can result in damage to the oculomotor nerve. In addition, it is difficult to properly position the metal splint as it is close to the proximal aspect of the fibula.
Similar patents RU2654593C1
- Gilev Mikhail Vasilyevich
- Yuri Valeryevich Antoniadi
- Elena Alexandrovna Volokitina
- Dmitry Chernitsyn
- Dmitri Shiryakov
- Konovalov Yevgeny Alexandrovich
- Ruslan Valeryevich Saytsev
- Sayat Vitaly Viktorovich
- Komogortsev Igor Evgenievich
- Alkhashlamun Jabril Abdol Razak
- Epshtein Aliona Aleksandrovna
- Pritsov Alexei Petrovich
- Lazko Fyodor Leonidovich
- Zagorodny Nikolay Vasilyevich
- Shoemaker Vladimir Ivanovich
- Vadim Makushin
- Chegorov Oleg Konstantinovich
- Igor Yevgenievich Komogortsev
- Sergei Vyacheslavovich Zudayev
- Alhashlamun Jabril Abdol Razak
- Vladimir Chominets
- Roman Alexandrovich Fedorov
- Alexey Sergeyevich Grankin
- Oleg Vladimirovich Rikun
- Konokotin Dmitri Alexandrovich
- Igor Belenky
- Sergey Georgievich Semenov
- Aleksandr Yuryevich Kochish
- Sergeyev Gennady Dmitrievich
- Boris Mayerow
- Benin Andrei Vladimirovich
- Sergei Gennadyevich Kuvzhinov
- Vlasov Maxim Valeryevich
- Tenilin Nikolai Alexandrovich
- Vladislav Sergeyevich Strakhov



Causes of Osteophytes
- Degeneration (aging) and loss of bone density
- mechanical damage
- instability of the joint
- Osteoarthritis (inflammation of the subchondral bone)
- Calcium metabolism disorders (hormonal and metabolic disorders)
- systemic pathologies
- familial inheritance (genetic mutations)
- extrapulmonary tuberculosis and other specific chronic infections
In some cases, osteophytes of the knee joint are caused by neoplastic and metastatic processes.
Symptoms of bony hypertrophy of the articular surfaces
Osteophytosis of the knee joint is not a disease, but a radiological sign characteristic of arthrosis. In the early stages, the osteophytes appear as small prongs 1-2 mm long. With the progression of the pathological process, they increase in size, take on different shapes and lead to a narrowing of the joint space, an increase in the size of the condyle and socket of the knee joint.
Changes in the number and size of bony outgrowths are a typical marker of disease progression. The absence of any radiological evidence of osteophytes in the knee joint indicates the success of the treatment. When bony outgrowths are present, patients complain of difficulty bending and extending the knee and pain with movement. In advanced cases, the pain persists even at rest, and there is swelling and deformation of the joint. If the osteophytes press on nerve structures or are deeply embedded in muscles, the disease progresses.
Causes of osteonecrosis
As previously mentioned, osteonecrosis occurs when the blood supply to a specific area of bone tissue is imbalanced. In this case, the lack of nutrients leads to degeneration and the so-called collapse of the articular cartilage, which leads to the development and further progression of osteoarthritis.
Septic (avascular) necrosis of the knee joint is typical in patients who use hormone therapy for a long time, with alcohol abuse and in some cases also after trauma.
In addition, the experts also distinguish the so-called spontaneous osteonecrosis, the etiology of which has not yet been clarified and which is characterized by severe pain in the knee area.
The risk group usually includes people over 60 years of age, most of them women.
risk factors
The exact cause of an imbalance in the blood-bone system is often difficult to determine. However, doctors call the following risk factors that, in one way or another, can affect the development of the disease
- Knee dislocation, stress fractures and other types of trauma leading to vascular damage;
- sickle cell anemia, obesity, lupus erythematosus;
- regular use of corticosteroids, e.g. B. in rheumatoid arthritis, bronchial asthma, etc. It should be noted that it is currently not known exactly how steroids can affect the development of osteonecrosis, but a direct link with this group of drugs is evident;
- Excessive and prolonged consumption of products containing alcohol;
- transplantation of donor organs, etc.
However, early diagnosis of osteonecrosis and the lack of proper treatment almost certainly lead to severe osteoarthritis.
Conservative treatment
Conservative treatment includes immobilization with a cast or orthosis and restricting movement and weight bearing on the leg. During this treatment, the doctor will take x-rays at regular intervals to assess bone fusion. The mobility of the knee joint and the load on the leg depend on the type of fracture and the treatment chosen.
There are several methods that allow the surgeon to restore the correct position of the bone fragments and keep them in that position until they heal.
Internal' fixation. In this procedure, the bone fragments are first placed back into their normal position. They are held in this position by special fixators - intramedullary rods or plates and screws.

(Left) fracture of the proximal end of the tibia. (To the right) The same type of fracture secured with an intramedullary pin.
For fractures of the proximal quadrant of the tibia, when the fracture line does not penetrate the joint, both a rod and plate can be used. The rod is inserted into the intramedullary canal in the center of the bone and the plate is attached to the outer surface of the bone with screws.
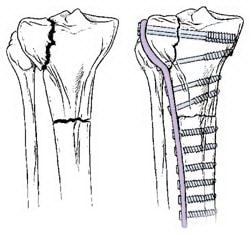
Fractures that penetrate the joint usually need to be stabilized with a plate. The plate is attached to the outer surface of the bone.
For fractures that penetrate the joint, plates and screws are typically used. If the fracture is associated with an indentation in the joint surface, that area must be repaired to restore normal joint anatomy and function. A bone defect is then usually created at the fracture site. Such cavities are filled with bone material taken from the patient himself or from a bone bank. Synthetic or natural products to stimulate bone regeneration can also be used.
pain relief
After the surgery you will experience some level of pain. This is an essential part of the healing process. The doctor and nurse will do everything they can to reduce the intensity of the pain, thereby speeding up your recovery.
Various drugs are used to relieve pain in the postoperative period: opioids, nonsteroidal anti-inflammatory drugs and local anesthetics. To maximize their effects and reduce the need for opioid analgesics, these drugs can be prescribed in various combinations with each other.
It's important to remember that while opioids are effective in controlling post-operative pain, they are narcotics and can be addictive. Drug addiction and overdose have long been a societal problem in most industrialized countries. Opioids may only be taken with a doctor's prescription. As soon as the pain syndrome subsides, it is better to stop them. If this doesn't happen within a few days of surgery, you should discuss the issue with your doctor.
causes of injury.
Causes include indirect injuries such as falls from a great height onto an outstretched leg, sports in which the leg is stationary and the torso and hip are rotated (skiing, soccer, speed skating), etc.
- acute knee pain
- Swelling and sudden enlargement of the knee joint
- Inability to move the knee joint at all.
- Bleeding into the joint cavity (hemarthrosis) can occur
- ACL tears can lead to drawer symptoms (unnatural rolling forward and backward of the lower limbs).
diagnosis of the injury.
- Examination of the injured person by a trauma surgeon.
- Mandatory X-ray examination (normal and lateral X-rays)
- Computed Tomography
- MRI
- Arthroscopy (in case of suspected cruciate ligament, meniscus of the knee)
Treatment for such an injury depends on the severity of the fracture. Conservative treatment is recommended for injuries without fracture displacement and for fractures of the intercondylar process:
- Puncture of the joint (removal of blood and fluid accumulations in the knee joint, injection of an anesthetic solution)
- Immobilization of the limb with a plaster splint (for 1.5-2 months).
- After this period, rehabilitation treatments are recommended.
If the displacement of the fragment is very large, surgical treatment with removal of the fragment or immobilization with an interarticular splint is indicated. The fragment is removed and fixed with sutures.
Functions of the PCC
- Primary limitation of anterior tibialis dislocation: 85 % resistance on the anterior drawer test when the knee is held in 90 degrees of flexion.
- Secondary limitation of tibial rotation and varus angulation: valgus when the knee is in full extension.
- Proprioceptive function: presence of mechanoreceptors in the ligaments.
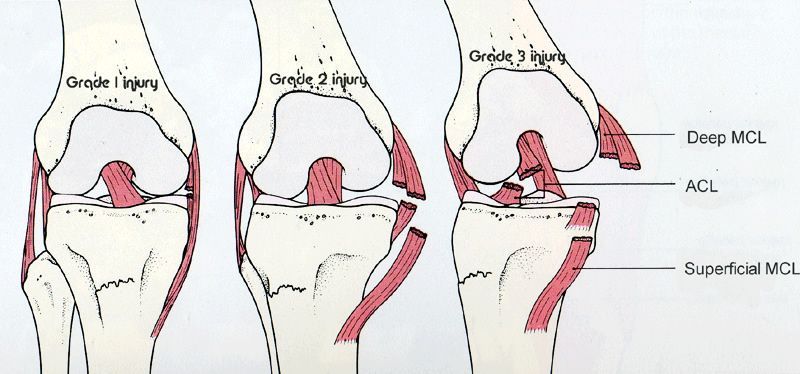
ISS injuries (Grade I-III) pose a particular challenge as they result in post-injury stiffness in the knee. Most orthopedists initially treat the MCI injury (for six weeks) with a knee brace to limit mobility. During this period, the athlete goes through a comprehensive rehabilitation program. Only then is an ACL reconstruction performed.
Bone contusions and microfractures
A subcortical tear of the trabecular bone (bone contusion) can result from the pressure exerted on the knee during a traumatic event and is particularly associated with a torn ACL. Concomitant meniscal and ISS injuries usually exacerbate the progression of bone contusion. Focal signal abnormalities in subchondral bone observed on MRI (not visible on radiographs) are believed to be microfractures, hemorrhage, and edema without disturbance to adjacent areas or articular cartilage. Bone contusions can occur independently of ligament or meniscus injuries.
Hidden bone injuries were found in 84-98 % of the patients with a torn PCC. Most have lateral compartment injuries affecting either the lateral femoral condyle, the lateral tibial plateau, or both. Although most bone injuries resolve, irreversible changes can remain. The literature is unclear about how long these bone lesions persist, but it has been reported that they can persist for many years on MRI. Rehabilitation and long-term prognosis may be uncertain in patients with extensive bone damage and associated articular cartilage damage. In cases of severe bone impingement, it is recommended to delay the return to full weight bearing to prevent further destruction of the subchondral bone and further aggravation of the articular cartilage damage.
diagnostic procedures
An accurate diagnosis can be made by the following procedures:
Physical examination, which includes the following tests:
Radiological examination.
If an ACL tear is suspected, radiographs of the knee joint should be taken in straight, lateral, and patellar views. The standing, propped view allows an assessment of the joint space between femur and tibia. It also enables the intertrochanteric indentation index to be measured, which provides important prognostic values for ACL tears. The patellar tendon and its height are measured on a lateral x-ray. Tunnel vision can also be helpful. The Merchant X-ray not only shows the joint space between the femur and the patella, but also helps determine if the patient has a dislocated patella. X-rays should note the following:
The intercondylar indentation index is the ratio between the width of the intercondylar notch and the width of the distal thigh at the level of the popliteal fossa, measured on a tunnel view radiograph of the knee joint. The normal intercondylar indentation index is 0.231 ± 0.044. The intercondylar indentation index is greater in men than in women. In athletes with non-contact PCC injuries, the incision width index was found to be at least 1 standard deviation below the mean, meaning someone with a PCC injury is likely to have a small incision width index compared to the norm. This is measured with a ruler parallel to the joint line. The narrowest point of the notch is measured at the level of the ruler. In more chronic ACL injuries, there may be reduced intercondylar eminence, hypertrophy, or osteophyte formation at the patellar margin.
This is also one of the reasons women are more prone to ACL injuries than men. It was also observed that the internal angle of the lateral femoral condyle was significantly higher in female athletes with a PCC tear than in female athletes without a PCC tear. The width of the intercondylar notch was statistically smaller in female athletes with an ACL injury than in non-injured female athletes. In addition, it was found that the internal angle of the lateral femoral condyle was a better predictor of ACL rupture in young handball players than the width of the intercondylar notch.
Types of aseptic necrosis of the femoral condyle
In the development of aseptic necrosis of the femoral condyle, four stages can be distinguished, each with characteristic clinical signs.
- The first stage is characterized by microscopic changes in the cartilage tissue that do not cause any external symptoms.
- In the second stage, the patient experiences discomfort when walking, sitting or standing for a long period of time.
- The third stage is characterized by severe pain that occurs with movement and hardly subsides at rest.
- The fourth stage is accompanied by severe necrosis of cartilage and bone tissue, which is manifested externally by severe pain and complete loss of joint function.
symptoms of necrosis
The main symptom of aseptic necrosis of the lateral and medial condyles is pain, which is initially localized in the knee and, as the pathology progresses, spreads to the hip and groin. The discomfort and discomfort are significantly worse with physical activity: walking, running, cycling, squatting. Over time, the pain begins to bother the patient even at rest or during sleep.
A characteristic symptom of the disease is morning stiffness, which can last for more than an hour with extensive lesions. An additional symptom is lameness and the resulting change in gait.
- Necessity of fibula fixation in tibia fractures 2016.02.05 Necessity of fibula fixation in tibia fractures
- Cartoon of Orthopedics Kiev, Ukraine 02.07.2015 Cartoon of Orthopedics Kiev, Ukraine
- Treatment of dislocation of the sternum end of the clavicle 2014.10.29 Treatment of dislocation of the sternum end of the clavicle
- Treatment of a luxated clavicle 2014.10.29 Treatment of a luxated clavicle 2014.10.29 Treatment of a luxated clavicle
- Treatment of fractures of the lateral end of the clavicle 2014.10.29 Treatment of fractures of the lateral end of the clavicle
- Intracranial internal fixation of collarbone fractures 2014.10.29 Intracranial internal fixation of collarbone fractures
- Treatment of diaphyseal fractures of the clavicle 2014.10.29 Treatment of diaphyseal fractures of the clavicle
- Treatment of clavicle fractures and dislocations of adjacent joints 2014.10.29 Treatment of clavicle fractures and dislocations of adjacent joints
- Postoperative management of scaphoid fractures 2014.10.29 Postoperative management of scaphoid fractures
- Surgical approach in the treatment of scaphoid fractures 2014.10.29 Surgical approach in the treatment of scaphoid fractures
Home ' How to get there ' Lower Limb Fractures ' Treatment of Fractures of the Tibia ' Treatment of Fractures of the Tibia Condyle.
In case of significant hemarthrosis the joint is punctured, the blood is drained and a novocaine solution is injected into the joint. If necessary, the puncture can be repeated.
Treatment of tibial condyle fractures without dislocation. Stretching and immobilization treatment is possible. In the extension treatment, a system of constant adhesive tension is applied to the tibia and femur in a moderate physiological position of the limbs. Therapeutic exercises are started after 3-4 weeks. The duration of traction is b-8 weeks. A metered load is allowed after 2.5-3 months, taking into account the plane of the fracture, the axis of the limb and the weight of the patient. Functionality returns after 3.5-5 months.
symptoms
The symptoms of the complaint are quite symptomatic:
- pain at the site of the lesion;
- hemarthrosis;
- visible deformation;
- impairment of the function of the joint;
- lateral mobility of the knee;
- impaired blood circulation;
- significant enlargement in the area of the knee;
- restricted habitual movement;
- with a fracture dislocation, a significant lateral deviation of the tibia.
If the person affected notices the above symptoms, an immediate medical consultation is required.
diagnosis
The traumatologist conducts a visual examination of the patient and collects the medical history. To confirm the diagnosis, the patient is referred for an X-ray in front and back projection. This technique shows the nature of the fracture and the displacement of the fragments.
The treatment technique depends on the depth of the problem. After anesthesia and final diagnosis, the doctor selects a treatment technique.
If there is no dislocation, the following techniques are used:
- The joint is punctured under local anesthesia;
- A plaster cast is applied for stabilization;
- After a period of time, massage and physiotherapy are recommended.
If there is a dislocation, the doctor will do a closed reduction, followed by skeletal traction.
If the fragments are dislodged, surgical intervention is required. The surgeon places the fragments in place and fixes them with metal fixtures. In the case of multiple fragments, an Ilizarov apparatus is used.
Physical activity is recommended according to an individual plan.
The described pain can be accompanied by unpleasant complications, such as: B. Deformations of the limbs, deforming arthrosis and arthrogenic contractures. They are all caused by inflammation, poor circulation and damaged innervation of the affected area.
Read more:- Osteophyte of the heel bone.
- Femoral collateral ligament.
- Displacement fracture of the heel bone.
- How long it takes for the ligaments to heal.
- tibia and fibula.
- Dislocation of a bone in a joint.
- Injury of the tibial condyle.
- Axis of rotation of the knee joint.
