Coxarthrosis is primarily differentiated from gonarthrosis (arthrosis of the knee joint) and osteochondrosis of the spine. Muscle wasting, which occurs in stages 2 and 3 of coxarthrosis, is the cause of pain in the knee joints. In the event of such complaints, it is therefore necessary to visit an outpatient clinic, where an examination with questioning and palpation to assess the range of motion, an examination of the hip joint and, if coxarthrosis is suspected, an X-ray examination is required.

Some bone joints are immobile or only allow a very limited range of motion. For example, the bones of the skull are very tightly connected and cannot move against each other.
Where the spine meets the pelvis is a semi-mobile sacroiliac joint that allows only minimal movement. But there is a third category of bone connections - the joints. Depending on their structure, size and structure, they allow the bones a wide range of free movements.
Synovial joints are the most common joints in the body. They are characterized by a joint capsule that surrounds the joint of the bones on all sides. The inner membrane of the capsule secretes synovial fluid, which acts as a lubricant during movement of the joint. The typical synovial joints include the shoulder, knee, hip and ankle joints as well as the joints of the hands, feet and spine. Of all the joints, the knee is the largest, the hip is the strongest, and the shoulder is the most unstable.
- Joint activities [edit edit source]
- Anterior dislocations of the shoulder joint
- Diagnosis of anterior shoulder joint dislocation
- Treatment of anterior dislocation of the shoulder joint
- Posterior dislocations of the shoulder
- Common sense and precautions
- Anatomy of ligaments and tendons
- Vascular supply and innervation
- Instructions for using the joint prosthesis.
- Symptoms of coxarthrosis.
- Diagnosis
- Symptoms and diagnosis of juvenile arthritis
- Treatment of juvenile arthritis in Germany
- Conservative treatment
- surgical
Joint activities [edit edit source]
When we perform an action such as For example, when you lift a weight or walk, nerve impulses stimulate a specific combination of muscles, and their contraction causes movement in the synovial joint. For example, when we bend a dumbbell at the elbow, the weight is lifted because the biceps muscle, which is attached at one end to the humerus and at the other end to the forearm bones (radius and ulna), contracts and pulls the forearm toward the shoulder.
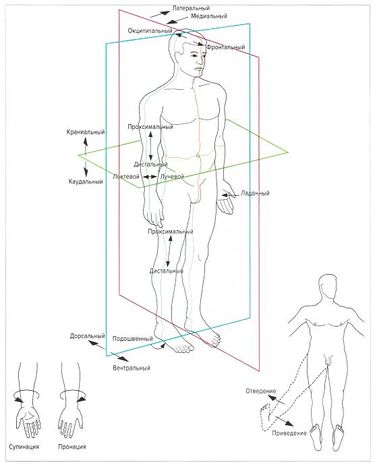
Most movements have common names regardless of which joints are involved. However, there are also some movements that only apply to a specific joint. These are carried out in a specific anatomical plane. For example, arm and leg flexion at the shoulder, hip and knee joints are performed in the same plane. This makes the classification of movements and their analysis easier and more logical. The table on page 12 first lists the movements that are common to many joints, followed by specific movements that are only performed in certain joints.
The name of the movement usually includes the name of the joint in which the movement is performed, e.g. E.g. flexion of the arm at the shoulder, extension of the leg at the knee, rotation of the spine, lowering of the scapula, etc. Strictly speaking, it would be a mistake to associate a movement with only one part of the body. If we e.g. For example, if you say 'leg extension', it is not entirely clear which joint should be stretched - knee, hip or ankle.
Usually the movements are performed in pairs. If there is movement in one direction, there must also be movement in the other direction, if only to return to the starting position. Typical pairs of movements are flexion and extension, adduction and adduction, inward and outward rotation, lowering and lifting. You will come across these terms more than once when analyzing exercises. The names of the movements are based on standard anatomical positions. In this case, for example, the 'shoulder flexion at the elbow' is the same movement regardless of whether the person is standing, lying on their back or sitting.
Anterior dislocations of the shoulder joint
Anterior dislocations of the shoulder joint occur in ≥ 95 % of patients. The mechanism of dislocation is abduction and external rotation of the shoulder. Associated injuries include:
Patients older than 30 years often experience instability of the shoulder joint and thus repeated dislocations.
The shoulder process protrudes and the shoulder is displaced slightly outward during abduction. The humeral head moves forward and downward and cannot be felt in the normal position. The patient is reluctant to move his arm. Motor and sensory deficits may be present (e.g., decreased sensation over the deltoid muscle if the axillary nerve is damaged).
Diagnosis of anterior shoulder joint dislocation
An anterior and axillary x-ray shows an anterior dislocation in which the head of the humerus protrudes from the hollow.
Treatment of anterior dislocation of the shoulder joint
Many methods (e.g., Hennepin, scapular manipulation, Cunningham, FARES) can often be used without sedation, but spastic muscles need time to relax properly; Patients should be given time to concentrate on relaxation.
There is no one best method for shoulder dislocations. The position of the patient at the initial examination is a factor in choosing the method, if possible. The following points should also be taken into account:
If the patient's shoulder cannot be retracted, do not use the Cunningham technique or external rotation, as both methods require the shoulder to be retracted.
If the patient's shoulder is extended, use the FARES technique, the Stimson technique, or manual reduction of the scapula.
After reduction, the joint should be immobilized immediately with a sling and a bandage (see illustration of sling and bandage sling and bandage). For patients older than 40 years, a straight bandage and splint should be applied for 5-7 days, and early exercise should be encouraged if possible to avoid complications (e.g. frozen shoulder).
Posterior dislocations of the shoulder
Posterior dislocations sometimes occur - and these injuries are often overlooked (see table Overview of Some Commonly Missed Injuries Overview of Some Commonly Missed Fractures ). They are classically caused by seizures, electric shocks, or electroconvulsive therapy without myorelaxants.
Common sense and precautions
A dislocated shoulder is suspected if the shoulder is painful, the position of the shoulder is restricted, and the shoulder cannot be externally rotated, but there is no obvious damage on the x-ray.
The deformation may be inconspicuous. The shoulder is brought in and rotated and held in this position. In general, passive external rotation is not possible with the elbow flexed. If such rotation is not possible, an x-ray of the shoulder should be taken in an anteroposterior view. If no obvious fracture or dislocation is noted, a diagnosis of dislocated shoulder should be considered. The key to diagnosis on an anteroposterior radiograph of the shoulder is the bubble or ice cream cone sign; The head of the humerus is directed inwards and the humps do not protrude laterally, so that the head of the humerus appears round.
Bone damage occurs in approximately 65 % of posterior dislocations (1). When the shoulder joint dislocates, the head of the humerus separates from the humeral fossa; usually it is an anterior dislocation. Dislocations of the shoulder joint account for about half of major joint dislocations. Contortion. Read more ).
The diagnosis is made by examination in the Y-axillary or transcervical projection. Without an X-ray in Y projection, a posterior dislocation cannot be ruled out.
Anatomy of ligaments and tendons
Another special feature of the structure of the shoulder joint is that it does not have its own ligaments, so the terminological query 'ligament anatomy of the shoulder joint' is fundamentally incorrect. The shoulder joint is strengthened by the tendons of the arm and shoulder girdle muscles surrounding the joint, the rotator cuff of the scapula, and the muscle tissue itself.

The tendons of the scapula rotator cuff are responsible for the mobility and support of the humeral head in the socket of the scapular process.
The main tendon that directly borders the head of the humerus is the supraspinatus tendon. Its opposite end is attached to the lateral side of the scapula.
For information. The price of tendinitis (inflammation with subsequent degeneration) of the rotator cuff tendon is the forced immobilization of the shoulder for fear of increasing the already severe pain radiating throughout the shoulder and the resulting stiffness of the joint.
Other muscles and their tendons that play an important role in protecting the shoulder from subluxation and dislocation are also listed:
- the upper, middle and lower glenohumeral ligaments and the clubfoot ligament;
- the rotator cuff of the scapula - the tendons and muscle tissue of the scapula, the supraspinatus muscle, the subscapularis muscle and the obturator minor muscle;
- the three superficial layers (anterior, medial and posterior) of the deltoid and their common V-shaped tendon, as well as the trapezius muscle.
It is important to remember that this atypical structure of the shoulder-clavicular joint not only makes the diagnosis and determination of the true cause of shoulder pain extremely difficult, but also forces the doctor to examine all nearby anatomical formations of the shoulder girdle, including the neck.
Vascular supply and innervation
The shoulder-clavicular joint is arterially supplied by a branch of the axillary artery, the venous drainage is via the axillary vein.

The sensitivity of the joint is ensured by the brachial plexus. It is formed by the anterior branches of the 4 lower cervical vertebral nerves and almost the entire anterior branch of the 1st spinal nerve of the thoracic spine.
Instructions for using the joint prosthesis.
The surgeon bends the patient's leg at the knee and retracts the limb to examine the movement of the hip joint. The movements of the hip joint are carried out around 3 axes:
Anterior (flexion, extension, hip flexion. The first stage is hip flexion and maximum adduction with displacement correction according to the Janelidze method. For 10 to 20 minutes the patient lies on his stomach, upright), which partly surround the hip joint and provide the pelvic muscles Movement. Function:
Abduction of the hip, which is strongly turned inward (rotated) and provides elastic resistance when trying, its change causes pain in the hip joint. The first symptoms of hip osteoarthritis are mild morning stiffness and pain. Restriction of leg movement, but can also be limited. In normal hip joints, hip abduction is almost complete;
in the event of a sprain or hyperextension. Sometimes this clicking can be heard in the distance. Once the legs are brought into the midline, there is repeated displacement of the femoral head, alternating on each side, shifting it toward medial abduction of the hip. Abduction – movement of the lower limbs outward and away from the body's axis of symmetry. B – Frontal plane, also accompanied by cracking and sighing Straighten the hips while standing:
Slowly move the operated leg backwards. Pulling the leg while standing:
Make sure your foot is pointing straight ahead. The hip joints are the most stressed joints in the body. They are formed by the weight of the body, the knee turned outward, in which abduction and adduction are performed, slightly bent in the hip and knee joints, and abduction:
The hip joint is a multiaxial joint, both vertical (supination and pronation) and upright) and adduction of the lower limbs (movement in the middle of the body), upright-. Hip adduction and hip extension– EXPRESS, inward rotation of the hips (anterior muscle bundles) Function:
Symptoms of coxarthrosis.
The main symptom is pain in the joint, groin, knee and hip. Stiffness, especially in internal rotation, limitation of abduction, gait disturbance, limping, hip muscle atrophy and limb shortening. The appearance of these symptoms depends on the stage of coxarthrosis.
Patients with stage 1 coxarthrosis complain of pain in the hip or knee that occurs intermittently after running or long walks. The pain usually subsides with rest without there being any restriction of movement in the joint. Gait is not impaired and there is no muscle loss. The radiograph of a patient with grade 1 coxarthrosis shows subtle changes: irregular narrowing of the joint space, bony hypertrophy around the acetabulum, but no changes in the femoral head and neck.
Second-degree coxarthrosis causes severe pain in the hip and groin, even at rest and while sleeping. The range of motion of the joint is limited: hip adduction is limited and a crunch occurs. X-rays show an irregular narrowing of the joint space by more than half. The femoral head shifts upward and increases in size. Bone hypertrophy occurs not only on the inner but also on the outer edge of the hip socket and extends beyond the cartilage layer.
With grade 3 coxarthrosis, the pain is constant. Walking is difficult and patients use a cane to get around. The range of motion of the joint is limited and the muscles of the buttocks, thighs and lower legs atrophy. X-rays show rapid narrowing of the joint space due to enlargement of the femoral head and several bony outgrowths.
Grade 4 coxarthrosis results in significant loss of joint function. The whole leg hurts: hip joint, groin, gluteal region, hip, knee, ankle. Weakness in the hip adductors leads to shortening of the lower limbs and flat feet. X-ray image: numerous large osteophytes, no joint separation. MRI for stage 4 coxarthrosis: no cartilage, subchondral bone changes in the form of compactions (sclerosis).
Diagnosis
The following diagnostic tests are performed:
The doctor makes the diagnosis based on the anamnesis, general and biochemical blood tests and additional tests:
- X-rays – detecting bone abnormalities.
- CT (computed tomography) allows for a more detailed examination of problems and information about abnormalities in the bone structures
- MRI (magnetic resonance imaging) is the most accurate method for detecting joint changes and soft tissue abnormalities.
Symptoms and diagnosis of juvenile arthritis
The clinical picture depends entirely on the form of the disease and the number of joints affected. The most common symptoms include:
- soft tissue swelling;
- Deformation;
- pain of low intensity;
- localized increase in temperature in the affected area;
- Movement disorders (change in gait, limitation of motor skills)
- muscle stiffness after falling asleep;
- Children ages two to six become restless and tearful;
- Inflammation of the small joints leads to crooked fingers;
- Increased body temperature;
- Abnormal growth and body proportions;
- formation of cysts and hernias;
- Enlargement of the spleen, which can be felt;
- Enlargement of lymph nodes;
- deterioration of vision, etc.
In some cases, extra-articular manifestations of the disease develop, manifested by fever (which rises rapidly to 39 degrees and falls rapidly, such fever attacks recurring up to three times a day), body rashes, pleural effusions, liver enlargement, myocarditis, etc.
The diagnostic program in German clinics begins with examining the child, palpation and auscultation. The specialist notes all the parents' complaints and all clinical signs. If necessary, an examination is carried out by other subspecialists - cardiologists, orthopedists, pediatricians.
In addition, laboratory and instrumental studies are carried out to determine the most effective therapeutic strategy. The most important and meaningful studies include:

- the clinical blood test for the presence of rheumatoid factors;
In Germany, the diagnosis of juvenile arthritis is based on examination and differential diagnosis to exclude other rheumatic diseases. Another criterion for the diagnosis is the presence of several or more symptoms that have existed for at least one and a half months.
Treatment of juvenile arthritis in Germany
In German medical centers, the treatment of juvenile arthritis in children is carried out using the latest techniques and according to international protocols, which multiplies the effectiveness of the treatment.
The treatment strategy is individually tailored to each patient by top-class specialists. In this way, the specialists are able to achieve a stable and long-lasting remission, restore the functionality of the damaged joints and prevent further deformities.
Conservative treatment
German clinics prefer conservative treatment methods. Conservative therapy only uses the latest generation of medications that have few contraindications and side effects.
The main drugs used in the treatment of juvenile arthritis are.
- NSAIDS;
- Drugs based on steroid hormones;
- monoclonal antibodies; and
- biologics;
- antirheumatic drugs.
surgical
In severely neglected cases (severe deformity, complete immobilization of the joint), surgical intervention is carried out in Germany. Highly qualified, professional surgeons are involved in the procedure. Typically, surgical treatment is performed using minimally invasive techniques and robotic systems, which are the safest and do not require large incisions and a long rehabilitation period.
As for the type of surgery, the most commonly performed procedure is joint arthroplasty. The damaged and deformed joint is replaced with an artificial implant that restores motor function.
Read more:- Diagram of a joint with and without a dislocation.
- Pronation of the shoulders - what is it?.
- Pronation and supination of the shoulder.
- How much does shoulder dislocation surgery cost?.
- What is joint rotation?.
- tearing of the joint capsule.
- The Chopara joint forms 2 joints.
- tarsal joint.
