There is no specific prophylaxis for lymphedema. It is important to identify and treat the underlying disease early enough and to monitor the disease progression clinically and laboratory-wise.
- Lymphostasis of the lower limbs
- Causes depending on the type of disease
- What is Lymphedema?
- What is the risk of elephantiasis?
- Causes of lymphatic congestion
- classification
- Causes of Lymphedema.
- Why 'SM Clinic'?
- Lymphatic congestion of the lower limbs in children
- What is lower limb lymphostasis?
- Instrumental methods of diagnosis
- therapy
- Types of surgical treatment
- causes
- symptoms
- Symptoms of lymphostasis at different stages
- complications
- Prognosis in lymphedema
- Common sense and precautions
- Main Points.
Lymphostasis of the lower limbs
Lymphostasis of the lower limbs is lymphedema caused by stagnation of lymph outflow in tissues. Visually you can see that the affected leg is enlarged and swollen. But let's talk about the symptoms in detail.
Symptoms of lower limb lymphostasis vary depending on the stage of the disease. In the first stage, the swelling is mild and reversible. It usually occurs in the evening and is localized around the toes, around the ankles and on the back of the foot. The tissue remains quite soft, but by morning these symptoms will disappear and the foot will appear normal.
In the second stage, the swelling is irreversible. This means that it does not recede in the morning but keeps its shape steadily. The connective tissue grows, and the swelling itself gradually increases. All of this can drag on for years, with the situation getting worse and worse. Finally, the skin over the swelling can no longer be closed into a fold. Discomfort, heaviness and pain appear. Wounds or ulcers can form in places where the skin has come into contact with clothing and friction, causing lymphatic drainage. In addition, the skin takes on a bluish tint.
The third stage is called elephantiasis and is the most severe stage of the disease. It is characterized by dangerous complications: fibrosis, ulcers of various types, loss of limb contours and much more. All this affects the patient's physical abilities as well as his mental state.
There are also more general symptoms of lower limb lymphostasis. These include severe fatigue, weakness, headaches, significant weight gain (up to and including obesity), and joint pain. Due to the physical and mental stress, the ability to concentrate decreases, the distractibility increases and simple tasks become more difficult to complete.
In this case, of course, it is better not to reach the third stage and seek medical help as soon as possible.
Causes depending on the type of disease
Since there is a primary and secondary variant of the disease, the causes of lower limb lymphostasis largely depend on the type of disease.
The primary disease is a congenital problem caused by the small diameter of the lymphatic vessels, their abnormalities, underdevelopment of the lymphatic system, and various other factors.
When we speak of a secondary disease, it means that factors accumulated over the years have influenced its development. The causes of lymphatic stasis in the lower limbs are then as follows:

- Damage to the lymphatic system as a result of various injuries, including dislocations, fractures;
- formation of burn scars (scars must affect the lymphatic system);
- certain cardiovascular diseases;
- tumors of the lymphatic system, both malignant and benign;
- rye and other inflammatory conditions;
- Infections with certain parasites that invade the lymphatic vessels;
- surgery to the chest or chest;
- various pathologies related to kidney function;
- Bed rest that extends over a long period of time and is accompanied by immobility of the patient.
The causes of lymphatic congestion in the lower limbs are always due to lymphatic congestion, which contributes to the formation of further edema. Regardless of the cause, the patient in any case needs specialist medical help, comprehensive examination and treatment.
What is Lymphedema?
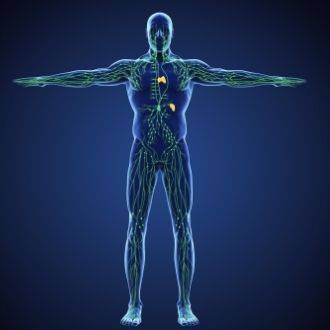
The lymph is referred to as the 'liquid tissue of the body'. It is an intercellular fluid that contains proteins and metabolic waste products and is involved in metabolism, immune responses, etc. Lymphatic circulation passes through the lymphatic vessels, and when it is disturbed, the fluid accumulates in the tissues. The causes of the disorders can be varied: congenital peculiarities of the lymphatic vessels and lymph nodes, trauma, operations, infectious diseases, obesity, tumors, etc.
In the early stages, lymphedema is difficult to recognize: it occurs in the evening and subsides after a night's rest. The limbs are soft to the touch and can be confused with edema that occurs after physical exertion. As the disease progresses, the lymphedema enlarges and becomes persistent and dense. The skin around the second toe cannot be folded (positive Stemmer's sign). The swelling starts at the foot and spreads up the leg.
When the disease reaches the third stage, doctors speak of elephantiasis or elephantiasis. The problem is that one leg is very different in size from the other (if the lymphedema affects only one limb), it is difficult or impossible for the patient to get dressed and move about. The swelling becomes dense because the lymph contains a lot of protein, and the protein molecules penetrate the tissue and form fibers there. Elephantiasis is accompanied by the appearance of warts and blisters on the skin, from which lymph can ooze.
What is the risk of elephantiasis?
Lymphedema, leading to tissue malnutrition in later stages. Ulcers, eczema or bacterial infections can appear on the leg. The limbs become greatly, sometimes critically, enlarged, making movement difficult. The result is gradual muscle wasting.
Lymphedema must be treated, otherwise the disease will progress and the condition will worsen. Lymphedema is one of those diseases that will not go away on its own! Self-medication is also dangerous, so these patients should be monitored by a doctor.
A combination of measures is required to reduce swelling and keep the limbs in good condition:
- manual lymphatic drainage massage
- instrumental lymphatic drainage massage
- Compression therapy (wearing special knitwear and bandages).
In addition, special skin care that reduces the risk of or helps manage infections, as well as physical activity and diet are required.
Treatment of the disease at the stage of elephantiasis is different. If the skin is inflamed, blisters form, and lymphatic congestion (lymphatic drainage) is noted, these disorders are first treated with appropriate topical medications and dressings. The swelling can only be treated once the skin lesions have healed. As the disease progresses, surgery is sometimes done to remove some of the affected tissue.
It should be noted that late stage lymphedema is very difficult to treat and while the condition may improve, the leg often cannot be restored to its former size. The difference in volume of the limbs and the difficulties associated with them remain. So if you suffer from regular leg swelling that gradually gets worse, you should see a doctor who will make a comprehensive diagnosis and determine the cause of your condition. If necessary, he will prescribe you a treatment that can be successfully carried out in the clinic of the Phlebological Center.
Causes of lymphatic congestion
Lymphatic congestion can be caused by a number of factors. Disorders of the lymph circulation with lymph accumulation in the tissue in heart failure, kidney diseases, hypoproteinemia, when the lymph channels cannot cope with the lymph drainage. Lymphatic congestion can be the result of chronic venous insufficiency in decompensated varicose veins, postthrombotic syndrome and arteriovenous fistulas. The removal of excess tissue fluid leads to a compensatory expansion of the lymphatic vessels, reduced tone, valve insufficiency and lymphatic insufficiency.
Lymphatic congestion can be caused by malformations of the lymphatic system, obstruction of the lymphatics due to damage (mechanical and surgical trauma, burns), compression by tumors, or inflammatory infiltrates that prevent lymphatic drainage. In the case of lymphangitis and lymphatic vasculitis, the obliteration of a lymphatic vessel leads to dilation and failure of the valves of other vessels, which is associated with lymphatic congestion.
Extensive mastectomy for breast cancer is complicated by the development of upper limb lymphedema in 10-40 % of cases. As a rule, when performing mastectomy, axillary lymphodectomy (axillary lymphadenectomy) is performed, that is, the removal of lymph nodes that form regional metastases. The likelihood of lymphostasis is directly related to the extent of axillary lymphadenectomy. Prostate cancer, lymphoma, axillary lymphadenectomy, radiation therapy, and regional lymphatic drainage can also produce lymphostasis.
In some cases, disturbed lymphatic circulation with lymphostasis is observed with recurrent streptococcal lymphadenitis (phlegmon, rhynchus) and parasitic infections. Lymphatic filariasis (elephantiasis, elephantiasis) transmitted by mosquitoes occurs in tropical climates. Symptoms of infection include lymph node involvement, lymphadenopathy, fever, severe pain, hypertrophy of the legs, arms, chest, or genitals.
classification
Primary and secondary lymphostasis can occur due to etiological factors.
- Primary Lymphostasis is characterized by failure of the lymphatic system due to congenital anomalies of the lymphatic system (hypoplasia, agenesis or occlusion of blood vessels, valvular defects, hereditary syndromes). Primary lymphatic congestion may affect one or both limbs; Lymphedema occurs in childhood and increases in adolescence.
- Secondary lymphatic congestion (secondary lymphatic congestion). Secondary lymphedema is caused by injury or disease in the originally normal lymphatic system. Secondary lymphedema is more likely to occur in a limb, usually at the level of the foot and lower leg, and is more likely to be post-traumatic or inflammatory.
Lymphedema occurs predominantly in women. Lymphostasis of the lower limbs develops in 91 % of the patients. Lymphedema that develops between the ages of 15 and 30 is referred to as juvenile lymphedema, and after 30 years as late lymphedema. Lymphedema develops in three phases:
Causes of Lymphedema.
Lymphedema can be caused by:
- Genetic underdevelopment of the lymph vessels (e.g. Nonne-Milroy-Meige syndrome – in addition to lymphedema there are also endocrine disorders and internal organ damage);
- functional incompleteness of the lymphatic vessels;
- absence of a valvular apparatus;
- delayed lymph outflow;
- Damage to the vessels through which the lymph flows.
Why 'SM Clinic'?
Diagnosis begins with an objective assessment of the affected limb. The doctor necessarily checks the Stemmer's sign, which is determined by the third stage of lymphedema. This is the inability to pinch a fold of skin over the big toe due to severe swelling of the skin and subcutaneous tissue.
After the clinical examination, further diagnostics are carried out. This can include the following methods:
- Multidetector CT angiography is a contrast-enhanced imaging of soft tissue structures that can be used to assess the distribution of lymph along the limbs, the condition of the lymph nodes, and the presence of fibrotic changes in the skin and subcutaneous fat layer. The examination includes an objective measurement of tissue density at each level according to the Hounsfield scale.
- Doppler limb ultrasound – confirms the presence of edema, determines its location (above or below the muscle fascia) and extent, and reveals fibrotic changes in the subcutaneous tissue. The Doppler examination assesses the type of venous blood flow and excludes causes that can be traced back to venous insufficiency.
Further laboratory and instrumental examinations serve to identify other causes that can provoke edema syndrome - renal and cardiac insufficiency, venous pathological processes, etc.
Lymphatic congestion of the lower limbs in children

The vast majority of cases of primary lymphostasis of the lower limbs are most common in girls and young women.. Slight swelling of the feet and lower legs, which subsides after a short period of rest in the early stages of the disease, can eventually lead to severe disabilities.
This article explains what primary lymphostasis is and why it occurs Lymphostasis in childrenand explains how to treat the disease.
What is lower limb lymphostasis?
Lymphostasis is a stagnation of lymph in the soft tissues (muscles and subcutaneous tissue), which leads to severe swelling. Over time, an immune response develops against an abnormal soft tissue protein in the lymph. The inflammation damages the cells that then form the connective tissue .. The soft swelling thickens and becomes irreversible. As a result, the affected leg enlarges and 'elephantiasis' develops. The quality of life deteriorates due to 'elephantiasis', leads to the development of trophic ulcers and in some cases to the development of malignancy.
Lymphostasis of the lower limbs in children arises from congenital underdevelopment of the lymphatic system. Deformed lymphatic vessels are characterized by thin, slightly stretchy walls and underdeveloped valves. 'Imperfect' vessels cannot drain the lymph from the muscles and subcutaneous tissue. While the lymphatic system can still cope with the stresses of early childhood, the lymphatic vessels can no longer fulfill their main function during puberty, during the turbulent hormonal changes. Therefore rapidly increasing swelling.. If treatment is not initiated as soon as possible, the swellings quickly thicken and 'elephantiasis' occurs.
Instrumental methods of diagnosis
Other diagnostic procedures are performed to help plan surgical procedures. An ultrasound examination of the veins helps to rule out venous pathology as the cause of the edema. The examination of the soft tissues is carried out to determine the nature of the changes in the subcutaneous tissue. Ultrasound examination shows accumulations of lymph in the subcutaneous tissue and thickening of the superficial fascia. In the case of lymphedema, free accumulations of fluid can be seen in the subcutaneous tissue. With the help of ultrasound, the effectiveness of conservative and surgical treatment can be assessed.
Lymphography is a method of contrast medium examination of the lymphatic vessels. A contrast medium is injected directly into a peripheral vessel and the movement of the contrast medium is observed under X-ray control. With lymphography, the degree of blockage of the lymphatic drainage is made visible. Lymphography is mandatory before planning any surgical intervention.
Lymphoscintigraphy is an isotopic procedure that can be used to determine the degree of lymphatic congestion and the condition of the lymph nodes. This method does not allow definitive determination of surgical tactics. We do not use them to prepare for surgical treatment.
therapy
Conservative treatment is indicated in the early stages of lymphostasis, when there are no obvious changes in tissue structures. In severe cases, it can also be performed after the operation. Phlebo- and angioprotectors (Antistax, Detralex, Troxevasin, Venoruton) are used for therapy. These preparations reduce vascular permeability, improve microcirculation and normalize metabolism in the vascular wall. Peripheral blood flow is restored by vasodilators - xanthinol nicotinate, trental.
Trophism (cellular nutrition of tissues) is normalized by taking enzymes (hyaluronidase). Treatment is supplemented with vitamins and immunostimulants. Diuretics are not used, since the reduction in blood volume can lead to metabolic disorders. With the simultaneous existence of bacterial and fungal infections, antibiotics and antifungal drugs are prescribed. Toxic ulcers and eczema are treated topically.
Treatment of lower limb lymphostasis includes bandages and the use of compression stockings. Massages with lymphatic drainage and physiotherapeutic treatments such as laser magnet therapy, pneumocompression machine and hydromassage have a good therapeutic effect. A calorie-restricted diet and limiting salt intake are essential. Therapeutic gymnastics, swimming and Nordic walking are helpful.
Types of surgical treatment
liposuction. Removal of the fibrotic subcutaneous tissue by suction. Indicated in benign connective tissue hyperplasia.
Dermatofasciolipectomy of the islet. Removal of the affected skin areas with fibrous tissue, fascia and subcutaneous fat. Several liposuctions are performed before islet dermatofasciolipectomy. The postoperative wound is closed with skin flaps that remain in the surgical area or are taken from other areas of the patient's skin.
Creation of lymphatic anastomoses. These are bypass operations to connect lymphatic vessels to veins to improve lymphatic drainage. They are used for secondary lymphatic congestion, which occurs primarily after irradiation of the lymph nodes or after a mastectomy. Lymphatic anastomoses have no effect on primary lymphatic congestion. The essence of the operation is to connect the vessels of the lymphatic channel to a nearby vein by creating thin microanastomoses.
tunnel construction. Creation of isthmas in the tissues affected by the lymphatic congestion to drain the accumulated lymph from the affected area. The diverted lymph is absorbed by the unaffected lymphatic vessels, resulting in relief from the swelling.
The temporary tunnels are special prostheses or spiral drains. Coils made of a special inert material or sections of subcutaneous veins are used to create permanent tunnels.
Tunneling is indicated in advanced lymphedema when other methods, as mentioned above, are not possible. The effect of tunneling is temporary.
In the case of primary lymphedema, a transplant of the lymphatic tissue complex is performed. The essence of the operation is that a flap of skin with fascia and healthy lymphatic vessels and nodes is transplanted to the affected area. This ensures lymphatic drainage through the intact nodes and vessels that serve as drainage.
Additional medication is administered after the operation. Anyone who has lymphostasis needs to be monitored by an angiosurgeon. The need for supportive therapy usually persists for life.
causes
In most cases, the development of lymphoma is caused by the following conditions:
- Infectious diseases that cause inflammation of the skin and subcutaneous tissue;
- Chronic venous insufficiency syndrome with thrombophlebitis and varicose veins;
- lymph node lesions and ductal stenosis;
- trauma and burns affecting the subcutaneous layer of cells;
- malignant diseases treated with radiation therapy;
- tumors in soft tissue;
- Penetration and growth of parasites in the structure of the lymphatic system;
- Heart and kidney disease that has caused persistent tissue swelling.

Exposure to one or more of these factors, in conjunction with the anatomical characteristics of the patient's body, leads to a disruption in the conduction and contraction function of the lymphatic vessels. They lose their ability to circulate lymph throughout the body, causing congestion. This condition is particularly dangerous in the lower limbs, where the lymph fluid flows in in large quantities under its own weight, but cannot be transported upwards through the contracting vessels.
Proteins, mucopolysaccharides and other organic substances are released from the lymph with prolonged congestion. These impregnate the vessel walls and disrupt their natural structure. Connective tissue rapidly forms in the blood vessels, narrowing their lumen and preventing the movement of lymph in the body.
symptoms
The first symptom of the disease is a pronounced swelling that rises from the toes through the ankle to the lower leg and thigh. The consequence of this:
- The limb loses its natural shape and becomes columnar;
- The skin is stretched, which causes uncomfortable pain for the patient;
- The joints become less flexible;
- The vein pattern on the limbs disappears; the skin becomes noticeably thicker and darker, and its texture resembles an orange peel.
Symptoms of lymphostasis at different stages
Depending on the severity of the symptoms, the following stages are distinguished:
- At the first stage, swelling occurs only under the influence of external unfavorable factors: long sitting or standing, increased drinking, heat, etc. Swelling often occurs in the evening;
- In the second stage of lymphedema, swelling occurs more frequently and the patient experiences severe pain and heaviness in the legs. The pressure on the skin leaves a clear dent that gradually recedes. Due to the swelling, the patient gains weight, and the skin becomes noticeably rough and loses its natural elasticity;
- In the third stage, the joints of the limb become immobile, the limb loses its natural shape, and signs of trophic ulcers appear on the skin, which can lead to sepsis and the gradual development of tissue necrosis.
complications
Left untreated and left untreated, lymphedema can be the cause of:
If the disease persists for a long time, symptoms of lymphoangiosarcoma can occur.
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call +7 (495) 775-73-60
Prognosis in lymphedema
Complete healing of lymphedema is usually not possible. Systematic treatment and preventive measures can relieve symptoms, slow or stop progression, and prevent complications.
Sometimes primary lymphedema is treated with surgical reduction and soft tissue reconstruction.
Fluid mobilization measures (eg, limb elevation, compression, massage, compression bandages, variable pneumatic compression)
Surgical treatment of primary lymphedema may include soft-tissue reduction (removal of subcutaneous fat and fibrous tissue) and reconstruction if background quality of life is markedly impaired.
When treating secondary lymphedema, the underlying cause of the condition is treated. Measures to mobilize fluid (complex edema therapy) can be used to reduce lymphedema. This includes:
Manual lymphatic drainage massage in which the extremity is lifted and massaged ('kneaded') towards the heart
Surgical reduction of soft tissue, repair of lymphatic anastomoses, and creation of drainage channels have been used, but the effectiveness of these techniques has not been studied in detail.
preventive measures Overheating, excessive physical activity, and wearing tight clothing (including tonometer cuffs) on the affected limb should be avoided. Skin and nails require careful care, and vaccination, phlebotomy, and insertion of venous catheters into the affected limb should be avoided.
Common sense and precautions
Avoid vaccination, phlebotomy, and intravenous catheterization of limbs affected by lymphedema.
For mucus and lymphadenitis, beta-lactamase antibiotics effective against Gram-positive organisms (e.g., dicloxacillin) should be used.
Main Points.
Secondary lymphedema (caused by obstruction or dysfunction of the lymphatic system) is much more common than primary lymphedema (caused by hypoplasia of the lymphatic system).
Elephantiasis (excessive hyperkeratosis of the skin of the limbs affected by lymphedema) is a severe manifestation of lymphedema, usually caused by lymphatic filariasis.
Treatment is unconventional but can relieve symptoms, slow or halt disease progression, and prevent complications from developing.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Read more:- elephant foot.
- Shoes for swollen feet.
- Why the legs are longer than the body.
- Anatomy of the ligaments of the lower limbs.
- foot of phot.
- How to enlarge the foot.
- The tarsal of the foot.
- Orthopedic footwear under IPR.
