There are also more complex classifications. These help doctors assess the degree of tissue damage and prescribe appropriate treatment. For example, the University of Texas classification takes into account the depth of the ulcer, the degree of disruption of tissue blood flow, and the severity of the infectious process.

- Foot radiography in Moscow
- indications
- Once OAP manifests itself, the process goes through four stages.
- diagnosis
- The differential diagnosis of OAP in the acute phase includes two main questions:
- symptoms
- Complications of diabetic foot
- diagnosis
- Treatment of diabetic osteoarthropathy
- How do you recognize the first symptoms of the disease?
- At 21st Century Medical Center we are ready to offer diagnostic and therapeutic assistance to patients suffering from this disease.
- Diagnosis
- Treatment of Charcot foot
- Classification of Charcot arthropathy
- Anatomical classification of the foot according to Charcot (Sanders LJ and Frykberg RG, 1991)
- Pathological classification of Charcot foot (Eichenholtz SN, 1966)
- Modified by Sella EJ and Barrette C. (1999)
- Symptoms of Charcot's disease
- Diagnosis of Charcot's disease
- Treatment methods for diabetic foot
- Prevention of diabetic foot syndrome
- Diabetic foot diagnosis
- Treatment of diabetic foot syndrome
Foot radiography in Moscow
X-ray examination of the foot – X-ray examination to assess the condition of the distal tarsal bones, metatarsal bones and the joints of the foot formed by these bones. In traumatology, this technique is used for fractures and fracture dislocations. In orthopedics, the procedure is used for flat feet, club feet, other congenital and acquired foot deformities, degenerative and dystrophic diseases. In oncology, the procedure is recommended for tumors of the foot bones and in abscess surgery if there is suspicion of spread of purulent processes to the bone tissue. The standard examination is performed in two (straight and oblique or straight and lateral) or three (straight, oblique and lateral) projections.
X-ray of two feet under weight (3 projections) (detection of longitudinal flatfoot for the recruiting office)
X-rays of small joints, small long and spongy bones (hands, feet, sternum, shoulder blade, collarbone, ribs)
X-rays of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
X-ray examination of small joints, small long and spongy bones (hands, feet, sternum, shoulder blade, collarbone, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, shoulder, collarbone, ribs)
X-rays of small joints, small tubular and cancellous bones (hands, feet, sternum, shoulder blade, collarbone, ribs)
X-ray examination of small joints, small tubular and cancellous bones (hands, feet, sternum, scapula, clavicle, ribs)
indications
In traumatology, the main indication for an X-ray of the foot is a fracture of the metatarsal bone. Less frequently, the technique is used in the diagnostic search for less common fractures of the tarsal bones and dislocations of the foot. In orthopedics, the diagnostic procedure is indicated for clubfoot, flatfoot, hallux valgus and other acquired and congenital deformities. In oncology and abscess surgery, examination is indicated for suspected tumors, bony lesions of the foot, deep panarisis, foot phlegmon and other purulent processes.
For the x-ray, the patient is placed on his back with his legs bent at the knees. The feet rest on the table surface. For an oblique X-ray, the patient is placed on their healthy side. The legs are bent. A pillow is placed between the knees so that the foot is at an angle to the table surface. In traumatology and orthopedics, lateral x-rays of the foot are rarely taken because the tarsal bones overlap in this projection and are difficult to see on x-ray images. Lateral projection is used to assess the condition of the arch of the foot or to detect fractures of the metatarsal bones. To perform the lateral projection, the patient lies on their side with their legs bent and the healthy leg brought forward.
Once OAP manifests itself, the process goes through four stages.
The first (acute) stage is characterized by swelling of the foot, mild hyperthermia and localized hyperthermia. Pain and fever are uncharacteristic. Destructive changes may not be visible on x-rays (only microfractures at this stage); Osteoporosis of the foot bones is detected.
Second stage (subacute): bone fragmentation and onset of foot deformity. As a rule, there is a flattening of the arch of the foot on the affected side. At this stage, the swelling and inflammation decrease. X-rays show fragmentation of the bony structures.
Third (chronic) stage: Marked deformation of the foot, spontaneous fractures and dislocations. The nature of the deformation depends on the location of the lesion. In typical cases, stress on the foot while walking results in a 'pressed foot' or 'limp foot' deformity. This is accompanied by a valgus deformity of the inner edge of the foot in the area of the tarsus and a beak-like deformity of the toes. X-rays show bone fragmentation, marked skeletal deformity, calcification of the periosteum and parosteum. The skeletal function of the foot is completely disrupted and in severe cases the foot can be compared to a 'bag of bones'.
Complications of the fourth stage: overloading certain areas of the deformed foot leads to purulent cavities; If these become infected, it can lead to cellulitis of the foot, osteitis and gangrene.
diagnosis
Due to the complexity of treating OAP and the fact that it is a rare disease in the population, patients with suspected OAP should be referred to the Diabetic Foot Center for diagnosis and treatment. The diagnosis of OAP is made on the basis of clinical presentation, history (minor trauma, surgery) and radiological signs corresponding to the stage. Very often this complication is misdiagnosed as lymphostasis, thrombophlebitis, foot cellulitis, etc. because general practitioners do not know enough about OAP. Differential diagnosis is most difficult in the acute phase, when premature initiation of appropriate treatment results in irreversible disability.
The differential diagnosis of OAP in the acute phase includes two main questions:
- Are the inflammatory changes bone lesions or should they be considered as an expression of another disease (cellulitis of the foot, acute thrombophlebitis, angina arthritis, rheumatic joint changes, etc.)?
- Are the radiographic signs of bone destruction non-infectious (OAP) or infectious (osteomyelitis) disease?
To answer the first question, x-rays of the feet are required (although in the acute phase only non-specific osteoporotic changes may be present). MRI and foot scintigraphy show microfractures, inflammatory changes and increased blood flow in the affected bones.
Biochemical markers of bone loss (hydroxyproline, deoxypyridinoline, collagen fragments, etc.) can be determined. Markers of bone remodeling that reflect osteoblast activity (i.e. osteosynthesis) (alkaline phosphatase isoenzyme, etc.) can be used for a similar purpose. However, the levels of these substances largely depend on the activity of bone degradation processes throughout the skeleton.
symptoms
Patients often go to the doctor and complain about wounds and cracks on one or both feet that are slow to heal. The duration of the sores varies: some people worry when they see the sores persist for several weeks, while others only see a doctor years later. The patient may complain of pain, but this symptom does not occur if sensitivity is severely reduced. The severity of the pain syndrome is also influenced by the degree of circulatory impairment and the severity of the infection.
Type 2 diabetes is particularly insidious. This form of the disease is often latent and causes only mild symptoms, and the patient may present to the doctor with a process in the foot area.
Depending on the stage and severity of the process, the patient may also experience the following symptoms
- decreased sensitivity in the feet;
- Unpleasant feeling of numbness, tingling;
- blisters on the skin of the feet;
- changes in the color and temperature of the skin;
- Red 'streaks' or 'spots' on the skin;
- Pain in feet.
If an infection has developed, body temperature may rise, chills may appear, and general well-being may deteriorate. Such patients need urgent medical attention.
Reserve time to call us back. We are open 24 hours a day, 7 days a week.
Complications of diabetic foot
Neurological disorders, vascular diseases and foot infections in diabetes can lead to dangerous complications:
- osteomyelitis – An infectious process that occurs in the bones.
- abscess – A cavity containing pus.
- deformities Foot.
- Diabetic osteoarthropathy (Charcot foot). – A disease that leads to the destruction of bones and joints. If not treated in time, it leads to irreversible disabilities. Charcot foot develops in four phases: 1 – inflammation-like picture: redness, swelling; 2 – Dislocations in the joints of the foot and fractures; 3 – Destruction of the joints and deformation of the foot; 4 – Occurrence of ulcers on the back of the foot.
- gangrene – This is tissue death caused by an infection. Amputation of the foot is often indicated.
diagnosis
Because diabetic osteoarthropathy is difficult to treat and is a rare disease in the population, patients with suspected OAD should be referred to a diabetic foot specialist for diagnosis and treatment.
The diagnosis of diabetic osteoarthropathy is made on the basis of the clinical presentation, history (minor trauma, surgery) and radiological signs consistent with the stage. This complication is often misdiagnosed as lymphatic congestion, thrombophlebitis, cellulitis of the foot, etc. because primary care physicians are unaware of diabetic osteoarthropathy.
Differential diagnosis is most difficult in the acute phase, when premature initiation of appropriate treatment results in irreversible disability due to significant impairment of foot function of the affected limb.
differential diagnosis Diabetic osteoarthropathy in the acute phase raises two main questions:
- Are the inflammatory changes the result of changes in the bone structures or should they be considered as an expression of another disease (foot phlegmatism, angina, acute thrombophlebitis, rheumatic joint changes, etc.)?
- Are the radiographic signs of bone destruction a non-infectious (OAP) or infectious (osteomyelitis of the foot) disease?
In the case of the first question, an X-ray of the feet is necessary (although in the acute phase only non-specific osteomyelitis-like changes may be present). MRI and scintigraphy of the foot skeleton show microfractures, inflammatory changes and increased blood flow to the affected bones.
Biochemical markers of bone loss (hydroxyproline, collagen fragments, deoxypyridinoline, etc.) can be determined. Markers of bone remodeling reflecting osteoblast activity (i.e., osteosynthesis) – bone alkaline phosphatase isoenzyme, etc. – can be used for a similar purpose. However, the concentrations of these substances are largely dependent on the activity of bone resorption processes throughout the skeleton.
Treatment of diabetic osteoarthropathy
In the acute phase, the aim of treatment is to stop the osteolysis processes and prevent pathological fractures and/or their continuation.
The most common mistake is prescribing vasoactive drugs. These drugs are indicated only in ischemic and neurosurgical forms of diabetic foot syndrome, while in diabetic osteoarthropathy they can increase the already excessive blood flow in the bone.
Treatment of diabetic osteoarthropathy consists of full weight bearing on the limbs in the acute phase until the inflammatory symptoms (swelling, local hyperthermia) have subsided. The relief ensures consolidation of the bone fragments and is more important than the medication. Without adequate offloading, the bone fragments are at risk of shifting and developing progressive foot deformity.
Bed rest is advisable for the first few days and weeks. After that, walking is only possible in a custom-made orthosis, which transfers a large part of the load from the foot to the lower extremity. Temporary relief from the orthosis can be achieved by wearing a tunic, which differs from the orthosis in its standard shape (commercially available) and looser attachment to the limb.
Once the swelling has subsided (usually after 4 months), the orthosis is gradually removed and the patient can walk in custom-made orthopedic shoes.
The standard method of offloading the limbs in diabetic osteoarthropathy in most foreign countries, especially in English-speaking countries (USA, Canada, United Kingdom, Australia, etc.), is the use of immobilization casts made of polymeric materials with plaster-like properties (Total Contact Cast). However, even if highly qualified personnel are available for this procedure, in 1 out of 10 cases this method carries the risk of skin damage (pressure ulcers) under the immobilization bandage.
In the acute phase of OAP, drugs that affect bone metabolism are used.
How do you recognize the first symptoms of the disease?
- A burning, itching feeling on the skin;
- Painful sensations in the foot;
- flaky, dry skin;
- occasional numbness;
- Changes in temperature and skin color on the foot.
Patients at risk include diabetics, especially those with decompensated diabetes and high blood sugar levels, smokers, and patients with severe atherosclerosis.
There are several types of diabetic foot syndrome. Symptoms can vary depending on the form of the disease.
- In the neuropathic form, the nerve fibers are affected. There is a tingling and burning sensation in the feet, temperature fluctuations in the limbs and a decrease in sensitivity. In advanced stages, ulcers appear on the skin.
- In the neuroischemic form, damage to the microvascular system occurs. This form is characterized by pain in the lower limbs, a drop in foot temperature and pallor. Inadequate treatment causes the tissue in the toes or foot to die.
- The osteoarthropathic form, also known as Charcot foot, involves destruction of the joints, resulting in curvature and deformity of the foot.
At 21st Century Medical Center we are ready to offer diagnostic and therapeutic assistance to patients suffering from this disease.
Diagnosis
- Collection of complaints, anamnesis, examination;
- Ultrasound examination of the vessels of the lower limbs (duplex ultrasound);
- laboratory diagnostics;
- assessment of the degree of impairment;
- X-ray, CT (computed tomography), MRI (magnetic resonance imaging);
- Microbiological examination.
Treatment is carried out by several specialists – angiosurgeon, podiatrist, endocrinologist, neurologist and dermatologist.
People struggling with this disease need to take special care of their own health. A comprehensive approach to treatment is important:
- control blood sugar levels and cholesterol levels;
- right nutrition;
- Do not smoke;
- Choosing appropriate clothing and shoes: cotton socks, shoes;
- regular foot self-examination;
- Be careful when cutting nails - do not cut them at the root or injure the skin around them;
- Visit to a specialist if an ingrown toenail, fungus or inflammation is detected;
- Hygiene of the lower limbs – daily showering, moisturizing cream;
- Examination by specialists: podiatrist, vascular surgeon, dermatologist, neurologist, endocrinologist.
You can make an appointment with our specialists via our 24-hour helpline.
Treatment of Charcot foot
At the Foot and Diabetic Foot Surgery Center, we perform foot reconstructions for Charcot arthropathy, restoring the foot's ability to support itself.
The surgical procedures are performed using 'immersion fixators' (screws and plates). In cases where the patient's foot deformity is complicated by the presence of a purulent focus of infection, external fixators (Ilizarov apparatus) are used.
Conservative treatment is carried out by an endocrinologist in a center with the option of an individually adapted relief cast (total contact cast).
Classification of Charcot arthropathy
According to the clinical manifestations of the disease, DOAP can be divided into two phases: acute (estimated duration 6 months) and chronic (after the acute phase).
The most commonly used anatomical classification was developed by L. Sanders and R. Frykberg in 1991.
Anatomical classification of the foot according to Charcot (Sanders LJ and Frykberg RG, 1991)
- I – metatarsophalangeal joints of the big toes;
- II – tarsal joints; and
- III – tarsal joints;
- IV – ankle joint,
- V – Calcaneus.
(+ incidence)
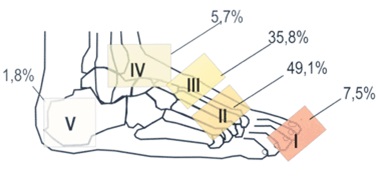
*Sanders L, Frykberg R. Diabetic neuropathic osteoarthropathy: the chenoid foot. In Frykberg RG, ed. The high risk foot in diabetes mellitus. 1991. p.325-333.
The radiological classification is based on the work of S. Eichenholtz, who in 1966 described the changes in the osteoarticular structure of the foot during DOAP as a three-stage process:
Phase I (development) is characterized by acute joint destruction
with subchondral fragmentation, diffuse osteopenia, ligamentous deformity and subluxation;
Phase II (consolidation) involves the resorption of most of the bone fragments and their consolidation with the underlying bone, thereby partially stabilizing the foot skeleton;
Phase III (reconstruction) is characterized by bone remodeling processes, subchondral osteosclerosis and osteophyte formation.
Pathological classification of Charcot foot (Eichenholtz SN, 1966)
0) Edema of the bone marrow
1) Fragmentation stage
2) Stage of merger
3) Stage of remodeling
*Eichenholtz SN. Springfield (Ill): Charles C. Thomas;. 1966.
Modified by Sella EJ and Barrette C. (1999)
0) Pain, swelling, hypersensitivity and hyperthermia over the joint;
1) Osteopenia, subchondral cysts, erosions, diastasis;
2) subluxations;
3) dislocation and destruction of the joint;
4) Healing and hypertrophy of bone.
Symptoms of Charcot's disease
Symptoms of Charcot-Marie disease appear at a young age, usually before the age of 20. The course is insidious and patients are able to function and take care of themselves for a long time. Causes that accelerate the progression of the disease can be viral and bacterial infections, unfavorable environmental influences, trauma, vitamin deficiency, etc.
In the ICD-10, Charcot-Marie-Tooth disease is coded as 'G60 Hereditary motor and sensory neuropathy', which somewhat corresponds to the clinical picture.
At the onset of the disease there is excessive fatigue, inability to stand in one place for long periods of time, numbness and 'goosebumps', followed by atrophic damage to the foot muscles, which is often symmetrical. The examination reveals a loss of tendon reflexes. The foot is so badly deformed that the patient can no longer walk on his heels. The atrophic process progresses to the lower legs and thighs.
The progression of Charcot-Marie-Tooth disease leads to involvement of the hands and forearms. The muscles of the neck, trunk and shoulder girdle do not atrophy. The proximal muscles are enlarged to compensate.
All types of sensitivities are affected, with superficial sensitivities being the most pronounced, particularly temperature sensitivity.
Diagnosis of Charcot's disease
A comprehensive examination is required to exclude diseases with a similar clinical picture. These include transverse amiosclerosis, myotonia and metabolic neuropathy. Muscle biopsies are performed to rule out chronic polyneuropathies.
All treatments for Charcot-Marie-Tooth disease are non-radical. Symptomatic treatment includes medication, physical therapy, treatment by an orthopedist, etc.
Physiotherapy for Charcot-Marie-Tooth disease includes physical therapy, massage, electrophoresis, diadynamics, mud therapy, baths, etc.
The aim of drug therapy is to improve the nutrition of muscle fibers. For this purpose, cocarboxylase, glucose, adenosine triphosphate, etc. are prescribed. Antioxidants, drugs to improve microcirculation and vitamins are also often used. Drugs that inhibit acetylcholinesterase activity and increase acetylcholine levels, e.g. B. Proserine and galantamine are well suited.
Further development of new drugs aimed at radical interventions is a world without Charcot-Marie-Tooth disease. The progression of Charcot-Marie-Tooth disease does not predict how long patients live.
At Yusupov Hospital, specialists have been helping patients keep the disease under control for years. The minimal severity of the symptoms and the slow progression are the result of the work of the doctors. In comfortable wards, with new equipment and in well-equipped rooms - this is where the treatment of Charcot-Marie-Tooth disease takes place. Do not delay your treatment, but make an appointment for a consultation.
Treatment methods for diabetic foot
- Antibiotic therapy: antibacterial agents, antibiotics, antiseptics. The choice of drugs and the duration of treatment depend on the results of blood tests and bacteriological examination of the wound contents
- Surgical treatment of ulcers: removal of the damaged tissue
- Relieving the burden on the affected limbs: using special devices and bandages
- Therapeutic measures to improve blood flow
- Physiotherapeutic methods: are mostly used after surgical treatment for rehabilitation purposes and consist of magnetic therapy, light therapy, UHF therapy, etc.
The most important thing that every diabetic should know is not to self-medicate, see a doctor in a timely manner and approach the matter holistically. Blood tests, treatment measures and a timely visit to a specialist can prevent tragic consequences.
Prevention of diabetic foot syndrome
Prevention of diabetic foot syndrome is important for people with diabetes.
- constant monitoring of blood sugar levels
- daily foot examination
- Avoiding bad habits (smoking, alcohol)
- Avoid walking barefoot, even at home
- Use of special orthopedic healing footwear
- Maximum protection against burns and hypothermia of the feet
- dietary treatment
- Carrying out therapeutic and breathing exercises (to improve the cardiovascular system, stabilize weight and improve lymphatic flow)
- regular medical checks
- Avoiding self-medication
Remember that it is much easier to prevent CVD than to treat it. If you undergo regular examinations and follow your doctor's advice, you can avoid unpleasant consequences and complications.
Article verified by: Dr. Andrei Vladimirovich Makhnev, chief physician of the Nanoaesthetic clinic, doctor of medical sciences, professor, surgeon of the highest category.
In the multidisciplinary medical center Nanoaesthetic, the podiatrist receives patients with diabetic foot syndrome. An appointment can be made online or by calling +7 (3452) 55-55-44.
Diabetic foot diagnosis
Patients at high risk of developing diabetic foot should be examined by an endocrinologist-diabetologist, a vascular surgeon and an orthopedist.
By improving diagnostic tactics, clinical examination and treatment of patients, the amputation rate can be reduced by 43-85 %.
The diagnosis of diabetic foot syndrome is made at the first surgical examination. The differential diagnosis between neuropathic and ischemic foot is mandatory.
Diagnosis of diabetic foot includes history of diabetes, examination of the feet to determine ankle-brachial ratio and reflexes, and assessment of sensitivity to touch, vibration, and temperature. In diabetic foot syndrome, special attention is paid to laboratory diagnosis - blood sugar, glycosylated hemoglobin, cholesterol, lipoproteins, sugar and ketone bodies in the urine.
In the case of ischemic diabetic foot, a comprehensive examination is carried out, which includes:
- Ultrasound of the vessels of the lower limbs - a method of detecting thickening and calcification of peripheral arteries and changes in blood flow velocity;
- X-ray contrast angiography and CT arteriography of peripheral arteries - methods for the accurate diagnosis of local vascular narrowings, which make it possible to choose the appropriate treatment for each patient.
- If osteoarthropathy is suspected, x-rays of the foot in 2 projections are possible,
- Bacteriological culture to determine the type of microflora and select appropriate antibiotic therapy in patients with foot ulcers.
Treatment of diabetic foot syndrome
People with diabetic foot syndrome should undergo a comprehensive physical examination, including an assessment of the condition of the feet, at least once a year. Early diagnosis is very important for timely treatment of the identified problems. Implementation of the recommendations and continuous follow-up care by a vascular surgeon, endocrinologist and neurologist will help prevent diabetic foot syndrome and prevent the development of complications.
To prevent complications of diabetic foot, it is important to maintain good blood circulation in the limbs. If treatment is initiated in a timely manner, medical revascularization is possible instead of surgery.
Drugs used in treatment include angioprotective drugs, antioxidants and antiaggregates. These are drugs that correct the properties of blood flow, strengthen the vascular walls, increase their elasticity and regenerate tissues. They have a general antispasmodic effect, cause vasodilation, improve microcirculation, normalize the rheological properties of blood and vascular permeability (increase capillary resistance), reduce tissue edema and activate metabolic processes in the blood vessel wall. The group of angioprotectors and antioxidants includes numerous drugs with different therapeutic effects: Pentoxifylline, Solcoseryl, Actovegin.
One of the best drugs to improve blood circulation in the lower limbs in diabetic angiopathy is vazaprostan. Treatment with vasaprostan improves the vascular bed - microcirculation and peripheral blood flow are improved.
Platelet aggregation inhibitors inhibit the clumping of blood platelets and erythrocytes and thus reduce their ability to stick to the endothelium of the blood vessels (adhesion). By reducing the surface tension of red blood cell membranes, they facilitate their deformation during capillary passage and improve blood flow. Antiaggregating agents can not only prevent aggregation, but also cause the disaggregation of already aggregated platelets.
Read more:- Charcot-Marie foot.
- Anatomy of the foot x-ray.
- What is Charcot?.
- Why amputate legs for diabetes?.
- Diabetic foot ulcers.
- Anatomy of the heel bone x-ray.
- Metatarsal amputation.
- Photo: Diabetic heels.
